|
Home
Bibliography
Calendar
Columns
Dorothy Brizill
Bonnie Cain
Jim Dougherty
Gary Imhoff
Phil Mendelson
Mark David Richards
Sandra Seegars
DCPSWatch
DCWatch
Archives
Council Period 12
Council Period 13
Council Period 14
Election 1998
Election 2000
Election 2002
Elections
Election
2004
Election 2006
Government and People
ANC's
Anacostia Waterfront Corporation
Auditor
Boards and Com
BusRegRefCom
Campaign Finance
Chief Financial Officer
Chief Management Officer
City Council
Congress
Control Board
Corporation Counsel
Courts
DC2000
DC Agenda
Elections and Ethics
Fire Department
FOI Officers
Inspector General
Health
Housing and Community Dev.
Human Services
Legislation
Mayor's Office
Mental Health
Motor Vehicles
Neighborhood Action
National
Capital Revitalization Corp.
Planning and Econ. Dev.
Planning, Office of
Police Department
Property Management
Public Advocate
Public Libraries
Public Schools
Public Service Commission
Public Works
Regional Mobility Panel
Sports and Entertainment Com.
Taxi Commission
Telephone Directory
University of DC
Water and Sewer Administration
Youth Rehabilitation Services
Zoning Commission
Issues in DC Politics
Budget issues
DC Flag
DC General, PBC
Gun issues
Health issues
Housing initiatives
Mayor’s mansion
Public Benefit Corporation
Regional Mobility
Reservation 13
Tax Rev Comm
Term limits repeal
Voting rights, statehood
Williams’s Fundraising Scandals
Links
Organizations
Appleseed Center
Cardozo Shaw Neigh.Assoc.
Committee of 100
Fed of Citizens Assocs
League of Women Voters
Parents United
Shaw Coalition
Photos
Search
What Is DCWatch?
themail
archives
|
GOVERNMENT OF THE DISTRICT OF COLUMBIA
OFFICE OF THE INSPECTOR GENERAL
SUMMARY OF SPECIAL REPORT: Emergency Response to the Assault on David E. Rosenbaum
CHARLES J. WILLOUGHBY
INSPECTOR GENERAL
OIG No. 06-I-003-UC-FB-FA-FX
June 2006
This Summary describes the D.C. Office of the Inspector
General’s review of the emergency response efforts provided by District agencies and hospital
personnel in light of applicable policies and procedures. The OIG is providing this Summary in
lieu of the full report in accordance with the exemptions provided in the District of
Columbia Freedom of Information Act (D.C. Code §§ 2-531-539 (Supp. 2004)) to preserve the
privacy interests of Mr. Rosenbaum and other individuals mentioned in the full report.
Table of Contents
Letter to the Mayor
Executive Summary
Background and Perspective
Scope and Methodology
Findings and Recommendations
Conclusion
Operations and Protocols of District Agencies and Howard
University Hospital
Office of Unified Communications
Fire and Emergency Medical Services Department
Metropolitan Police Department
Howard University Hospital
Office of the Chief Medical Examiner
Chronology of Events
Discovery of “Man Down” and 911 Call for Assistance
Office of Unified Communications Response
Universal Call Taker
Fire and Emergency Medical Services Dispatch
Metropolitan Police Department Dispatch
Issue and Finding
Did the Office of Unified Communications properly handle,
dispatch, and monitor the incident?
Recommendation
Fire and Emergency Medical Services Engine 20 Response
Engine 20 Arrives at Gramercy Street
Firefighter Interviews
Residents’ Observations
Issues and Findings
Did FEMS employees follow all rules, policies, protocols,
and procedures?
Did first responders properly assess the patient?
Were written reports and oral communication
adequate?
Recommendations
Metropolitan Police Department Officers Response
MPD Units Arrive at Gramercy Street
MPD Officer Interviews
Initiation of Assault and Robbery Investigation
Issue and Findings
Did MPD responders properly assess the situation at the
scene, and were steps taken by MPD responders prior to opening an
investigation adequate?
Recommendations
Fire and Emergency Medical Services Ambulance 18 Response
Ambulance 18 Arrives at Gramercy Street
Emergency Medical Technician Interviews
Issues and Findings
Did Ambulance 18 EMTs follow all rules, policies,
protocols, and procedures?
Did Ambulance 18 EMTs arrive with all due
and proper haste?
Did Ambulance 18 EMTs properly assess the patient?
Did Ambulance 18 EMTs select an appropriate hospital?
Were written reports and oral communication
adequate?
Are there any identifiable improvements to FEMS rules,
policies, protocols, and procedures?
Recommendations
Howard University
Hospital Emergency Department Personnel Response
Ambulance 18 Arrives at Howard University Hospital
Hospital Personnel Interviews
Issue and Findings
Did Howard University Hospital properly triage and assess
the patient upon his arrival at the hospital?
Recommendations
Office of the Chief Medical Examiner Response
Autopsy of David E. Rosenbaum
Issue and Findings
Did the OCME promptly and completely discharge
its review and report of the death?
Recommendation
Conclusion
Appendices
Appendix 1: Interviewees’ Contradictory Statements
Appendix 2: Map, Ambulance 18 Route to Gramercy Street
Appendix 3: FEMS Form 151 Run Sheet (not available online)
Appendix 4: Map, Ambulance 18 Route to Howard University
Hospital
Appendix 5: Ambulance 18 Log Sheet Entry (not
available online)
GOVERNMENT OF THE DISTRICT OF COLUMBIA
Office of the Inspector General
717 14th Street, N.W., Washington, D.C. 20005 (202)
727-2540
Inspector General
June 15, 2006
The Honorable Anthony A. Williams
Mayor
Office of the Mayor for the District of Columbia
1350
Pennsylvania Ave. N.W., Suite 600
Washington, D.C. 20004
Dear Mayor Williams:
In response to Mr. Bobb’s request that the Office of
the Inspector General (OIG) review the response to the January 6, 2006,
incident involving David E. Rosenbaum, please find enclosed our final
report. My Office reviewed the actions of the Office of Unified
Communications (OUC), the Fire and Emergency Medical Services Department
(FEMS), the Metropolitan Police Department (MPD), Howard University
Hospital, and the Office of the Chief Medical Examiner (OCME), regarding
their response to the incident.
In order to conduct this review, I appointed a team of
investigators and inspectors who have training and experience in law
enforcement, firefighting, medical care, and prehospital care. The team
reviewed policies, procedures, protocols, General and Special Orders,
personnel files, patient care standards, hospital and ambulance medical
records, certification and training records, and reports issued by FEMS,
MPD, the Office of the Chief Medical Examiner, and the Department of
Health. The team also interviewed all District government and Howard
University Hospital personnel involved in Mr. Rosenbaum’s emergency
care and the autopsy.
The OIG team concluded that, with the exception of OUC
and OCME, there was an unacceptable chain of failure in the provision of
emergency medical and other services to Mr. Rosenbaum as required by
FEMS, MPD, and Howard University Hospital protocols. Individuals who
played critical roles in providing these services failed to adhere to
applicable policies, procedures, and other guidance from their
respective employers.
These multiple individual failures during the Rosenbaum
emergency suggest alarming levels of complacency and indifference which,
if systemic, could undermine the effective, efficient, and high quality
delivery of emergency services to District residents and visitors. Our
review indicates a need for increased oversight and enhanced internal
controls by FEMS, MPD, and Howard University Hospital managers in the
areas of training and certifications, performance management, and oral
and written communications, as well as employee knowledge of protocols,
General Orders, and patient care standards. The OIG recommends, among
other things, that FEMS and MPD implement quality assurance programs
that would assign quality assurance responsibilities to the best-trained
or most senior employees dispatched to every medical and non-medical
emergency.
In order to give your office and the affected District
agency heads the clearest and most useful picture of the actions we
reviewed, this full version of the report contains the names of the
individuals involved, medical information, and sensitive personnel
information that should be handled securely. In addition, we are
enclosing a redacted version of the report without names and other
sensitive information, which will be available to the public on the OIG
website.
The significant concerns resulting from this review will
necessitate follow-up to our recommendations by the affected District
agency managers. So that I can be assured that our findings and
recommendations have been given the attention warranted, I request that
corrective actions that you require and receive from the agencies be
provided to me as soon as possible.
If you have questions about this report or if we can be
of further assistance, please feel free to contact me on (202) 727-9501.
Sincerely,
Charles J. Willoughby
Inspector General
CJW/ld
“Man Down.” On January 6, 2006, at approximately 9:20
p.m., a resident of Gramercy Street, N.W. went to his car to retrieve an
item and found an unknown man lying on the sidewalk in front of his
home. The resident’s wife called 911, and the Office of Unified
Communications dispatched emergency responders to the scene for a “man
down.” The fire (first responders), police, and ambulance (second
responders) personnel who were at the scene did not detect serious
injuries, illness, or evidence that the then-unknown man had been
physically attacked. He had no identification in his pockets, but was
wearing a wedding band and a watch. Stereo headphones were found near
him on the grass. Because he was vomiting, and because one or more
responders thought they smelled alcohol, the man was presumed to be
intoxicated. Consequently, the man was classified as a low priority
patient and transported to the Howard University Hospital (Howard)
Emergency Department where, after lying in a hallway for more than an
hour, medical personnel discovered that he had a critical head injury.
At approximately 11:31 p.m., Rosenbaum’s wife reported
to the Metropolitan Police Department (MPD) that her husband, David E.
Rosenbaum, had gone for an after-dinner walk at approximately 9 p.m.,
but had not returned. The police broadcast a descriptive lookout, and a
police officer who had responded to the Gramercy Street “man down”
call realized that the description of the missing person matched that of
the man who had been found lying on the sidewalk. It was later
determined that the “man down” was David Rosenbaum.
Mr. Rosenbaum’s head injury was discovered at Howard in
the early morning hours of January 7 and reported to MPD. MPD officers
then returned to the Gramercy Street scene to look for evidence that
might indicate the cause of the head injury. Later, on January 7, the
Rosenbaum family was alerted by credit card companies to unusual
activity on Mr. Rosenbaum’s credit cards. MPD subsequently linked Mr.
Rosenbaum’s injuries, his missing wallet, and the unusual credit card
activity, and initiated an assault and robbery investigation.
Despite surgery and other medical interventions to save
him, Mr. Rosenbaum died on January 8, 2006. The autopsy report issued on
January 13, 2006, by the Office of the Chief Medical Examiner concluded
that Mr. Rosenbaum was a victim of homicide due to injuries sustained to
his head and body.
Following Mr. Rosenbaum’s death, numerous questions
were raised and complaints made by both citizens and District government
officials about the emergency medical services provided to him by D.C.
Fire and Emergency Medical Services Department (FEMS) and Howard
personnel. Questions were also raised regarding the delayed recognition
by MPD officers that a crime had been committed.
In a letter to the Inspector General dated January 19,
2006, City Administrator Robert C. Bobb requested that the Office of the
Inspector General conduct a review of the response to David E. Rosenbaum’s assault and subsequent
death.1 Mr.
Bobb indicated that he and Mayor Anthony A. Williams wanted the review
“to ensure the maintenance of public confidence in the emergency
services provided by the District government.” In his letter to the
Inspector General, Mr. Bobb asked that the Office of the Inspector
General’s review specifically include answers to the following
questions:
- Did the Office of Unified
Communications properly handle, dispatch, and monitor the incident?
- Did FEMS employees follow all rules,
policies, protocols, and procedures?
- Did first responders properly assess
the patient?
- Were FEMS written reports and oral
communication adequate?
- Did MPD responders properly assess
the situation at the scene, and were steps taken by MPD responders prior
to opening an investigation adequate?
- Did the second responders arrive
with all due and proper haste?
- Did the second responders properly
assess the patient?
- Did the second responders select an
appropriate hospital?
- Are there any identifiable
improvements to FEMS rules, policies, protocols, and procedures?
- Did Howard properly triage and
assess the patient upon his arrival at the hospital?
- Did the Office of the Chief Medical
Examiner promptly and completely discharge its review and report of the
death?
In addition to Mr. Bobb’s questions, the Office also
received inquiries from Councilmembers Phil Mendelson and Kathy
Patterson regarding issues of concern with respect to this matter.
Finally, the Rosenbaum family requested that the Office of the Inspector
General answer questions they posed “so that errors [they] experienced
are not repeated in the future ….”
We believe that this report is responsive to many of the
questions that have been raised.
The scope of the Inspector General’s review included
the entire emergency response provided to Mr. Rosenbaum on January 6,
2006, and the review conducted by the Office of the Chief Medical
Examiner.2
To conduct the review, the Inspector General appointed a
team of inspectors and investigators to examine the circumstances
surrounding the January 6, 2006 incident. The team members have training
and experience in law enforcement, firefighting, medical, and pre hospital
care.3 The team reviewed policies, procedures,
protocols, General and Special Orders, personnel files, patient care
standards, hospital and ambulance medical records, certification and
training records, and reports issued by FEMS, MPD, the Office of the
Chief Medical Examiner, and the Department of Health. The team also
interviewed all District government and Howard personnel involved in Mr.
Rosenbaum’s emergency care and autopsy. Upon conducting its review,
the OIG team noted multiple discrepancies in statements made by
interviewees. (See Appendix 1)
Office of Unified Communications
- The Office of Unified Communications
properly handled, dispatched, and monitored the Gramercy Street call.
The call taker and dispatchers who handled the 911 call carried out
their duties appropriately.
Recommendation
None.
Fire and Emergency Medical Services Department
Engine 20
- Engine 20 personnel did not follow
all applicable rules, policies, protocols, and procedures. The
firefighter in charge of the Engine 20 crew on January 6 did not have a
current CPR certification as required. In addition, the
firefighter/Emergency Medical Technician (EMT) with the highest level of
pre-hospital training did not take charge of patient care during the
Gramercy Street call.
- Firefighter/EMTs did not properly
assess the patient. None of the firefighter/EMTs performed a complete
assessment of the patient, and not one of the patient’s vital signs4
was recorded at the scene. Once the firefighter/EMTs perceived an odor
of alcohol coming from the patient, they did not focus on other
possibilities as the cause of his altered mental status such as stroke,
drug interaction or overdose, seizure, diabetes, head trauma, or other
injury.
- Oral communication and standard
reports were not adequate. Firefighter/EMTs did not pass on key
information to the ambulance crew such as observing blood on the patient
and detecting the patient’s constricted pupils. Engine 20 personnel
did not prepare a written report on the Gramercy Street incident because
the FEMS form for such purpose is being revised.
Recommendations
- That FEMS ensure all personnel have current required
training and certifications prior to going on duty.
- That FEMS immediately implement a reporting form for
firefighter/EMTs who respond to medical calls so that first responder
actions and patient medical information can be documented.
- That FEMS develop and implement a standardized
performance evaluation system for all firefighters. The Office of the
Inspector General team determined that FEMS employees are not evaluated
on a regular basis, in the manner that other District government
employees are evaluated. Consequently, FEMS lacks standards to guide
firefighters’ performance and for use in evaluating their performance.
- That FEMS assign quality assurance responsibilities to
the employee with the most advanced training on each emergency medical
call. The designated employee should: (a) have in-depth knowledge of the
most current protocols, General Orders, Special Orders, and other
management and medical guidance; (b) monitor compliance with FEMS
protocols by all personnel at the scene; and (c) provide on-the-spot
guidance as required.
Metropolitan Police Department Responders
- MPD officers did not properly assess
the situation upon arrival. The three responding MPD officers did not
secure the scene, did not conduct an adequate preliminary investigation
in accordance with MPD General Orders, and did not take adequate steps
to determine if a crime had been committed. They also did not complete a
report on the incident pursuant to the relevant MPD General Order.
Recommendations
- That MPD immediately review and reissue the pertinent
General Orders relating to officer responsibilities at emergency
incidents. In addition, MPD should consider implementing or revising as
necessary a quality assurance program that includes supervisory review
of required reports, and a tracking system to ensure that reports are
written and retrievable for every call.
- That MPD assign quality assurance responsibilities to
the senior officer responding to each call.
Fire and Emergency Medical Services Department
Ambulance 18
- EMTs did not follow applicable
rules, policies, and protocols. The highest-trained EMT, an EMT-Advanced,
was not in charge of the patient as required by protocol. The EMT-Advanced
did not assess the patient, or help her partner assess him. Neither EMT
adequately questioned the first responding firefighter/EMTs about the
patient’s vital signs, or other care and treatment. The patient’s
low Glasgow Coma Scale results were disregarded, and not brought to the
attention of Howard Emergency Department personnel.
- The ambulance did not arrive on the
scene expeditiously. The ambulance driver got lost after being
dispatched from Providence Hospital, and then did not take a direct
route to Gramercy Street. This error added 6 minutes to the trip. (See
Appendix 2)
- EMTs did not thoroughly assess the
patient. The EMT who assessed the patient failed to conduct all of the
required assessments, and did not fully document his assessment and
treatment on the FEMS 151 Run Sheet. (See Appendix 3)
- Transport of the patient to the
hospital did not follow FEMS protocol. EMTs are required to transport
patients to the “closest appropriate open facility.” Although
Ambulance 18 was closest to Sibley Hospital, the EMT in charge, for
personal reasons, decided to transport the patient to Howard. Howard is
1.85 miles further from Gramercy Street than the Emergency Department at
Sibley Hospital. (See Appendix 4)
- EMTs did not properly document
actions. The EMT who cared for the patient did not completely fill out
the FEMS 151 Run Sheet. For example, the form shows no times when
treatment, care, or testing was provided or performed. An entire page of
the form relating to patient care was left blank.
Recommendations
- That FEMS ensure all personnel have current required
certifications prior to going on duty.
- That FEMS take steps to comply with its own policy on
evaluating EMTs on a quarterly basis.
- That FEMS promptly reassign, retrain, or remove poor
performers.
- That FEMS assign quality assurance responsibilities to
the most highlytrained pre-hospital provider for each incident. This
individual should: (a) have in-depth knowledge of the most current FEMS
protocols and other management guidance; (b) monitor compliance with
protocols and other guidance by all personnel at the scene; and (c) include
the results of on-scene compliance monitoring in all reports required by
management.
- That FEMS consider installing global positioning
devices in all ambulances to assist EMTs in expeditiously reaching their
destinations on emergency calls.
Howard University Hospital
- Nurses did not properly triage5 and
assess Mr. Rosenbaum. The triage nurse did not perform basic assessments
and did not communicate an abnormal temperature reading. The patient was
incorrectly diagnosed as intoxicated, but employees did not follow
triage policy on treating an intoxicated patient. Howard’s Patient
Care Standards—including monitoring airway and breathing, assessing
for trauma, conducting routine lab tests, and monitoring vital signs
every 15 minutes—were not followed.
Recommendations
- That Howard develop a system in the Emergency
Department that will allow staff to readily identify patients’
priority level while they are awaiting care.
- That Howard consider adopting a patient records system
that would enable nursing and medical staff to review documents when
they are at a patient’s side. The current system prevents staff access
to such information in a timely manner.
Office of the Chief Medical Examiner
- The Office of the Chief Medical
Examiner conducted the Rosenbaum autopsy expeditiously and promptly
issued a report.
Recommendation
- That Office of the Chief Medical Examiner consider using
digital camera technology to photograph all autopsies. The Office of the
Inspector General was unable to review requested autopsy pictures
because of photo processing delays and mislaid slides.
The OIG team concludes that personnel from the Office of
Unified Communications properly monitored the 911 call from Gramercy
Street and immediately dispatched adequate resources to respond to the
emergency. However, FEMS, MPD, and Howard personnel failed to respond to
David E. Rosenbaum in accordance with established protocols. Individuals
who played critical roles in providing these services failed to adhere
to applicable policies, procedures, and other guidance from their
respective employers. These failures included incomplete patient
assessments, poor communication between emergency responders, and
inadequate evaluation and documentation of the incident. The result,
significant and unnecessary delays in identifying and treating Mr.
Rosenbaum’s injuries, hindered recognition that a crime had been
committed.
On January 6, 2006, David E. Rosenbaum consumed alcohol,
both before and during dinner prior to leaving home for a walk.
Neighbors discovered Mr. Rosenbaum lying on the sidewalk in front of
their home and called 911. Upon assessment, emergency responders
concluded that Mr. Rosenbaum’s symptoms, which included poor motor
control, inability to speak or respond to questions, pinpoint pupils,
bleeding from the head, vomiting, and a dangerously low Glasgow Coma
Scale, were the result of intoxication. Hospital laboratory and other
tests, however, confirmed that Mr. Rosenbaum’s symptoms were caused by
a head injury. Emergency responders’ approach to Mr. Rosenbaum’s
perceived intoxication resulted in minimal intervention by both medical
and law enforcement personnel.
FEMS personnel made errors both in getting to the scene
and in transporting Mr. Rosenbaum to a hospital in a timely manner.
Ambulance 18 did not take a direct route from Providence Hospital to the
Gramercy Street incident. In addition, for personal reasons, the EMTs
did not take the patient to the nearest hospital. As a result of that
decision, it took twice as long for Ambulance 18 to reach Howard than it
would have taken to get to Sibley Hospital. Once FEMS personnel at the
Gramercy Street scene detected the odor of alcohol, they failed to
properly analyze and treat Mr. Rosenbaum’s symptoms according to
accepted pre-hospital care standards. Failure to follow protocols,
policies, and procedures affected care of the patient and the efficiency
with which the EMTs completed the call. In addition, FEMS employees’
failure to adequately and properly communicate information regarding the
patient affected subsequent caregivers’ abilities to carry out their
responsibilities.
MPD officers initially dispatched in response to the
Gramercy Street call failed to secure the scene, collect evidence,
interview all potential witnesses, canvass the neighborhood, conduct
other preliminary investigative activities, or properly document the
incident. Both FEMS and MPD failures were later compounded by similar
procedural failures on the part of Howard Emergency Department
personnel, who also initially believed Mr. Rosenbaum’s condition to be
the result of intoxication.
Upon Mr. Rosenbaum’s arrival at Howard, Emergency
Department personnel failed to properly assess his condition and failed
to communicate critical medical information to each other, thereby
delaying necessary medical intervention, all in violation of Howard’s
own patient care standards. Further, a number of Emergency Department
staff members passed Mr. Rosenbaum in the hallway and neglected to
provide clinical and therapeutic care.
The Office of the Inspector General’s review indicates
a need for increased oversight and enhanced internal controls by FEMS,
MPD, and Howard managers in the areas of training and certifications,
performance management, oral and written communication, and employee
knowledge of protocols, General Orders, and patient care standards.
Multiple failures during a single evening by District agency and Howard
employees to comply with applicable policies, procedures, and protocols
suggest an impaired work ethic that must be addressed before it becomes
pervasive. Apathy, indifference, and complacency—apparent even during
some of our interviews with care givers—undermined the effective,
efficient, and high quality delivery of emergency services expected from
those entrusted with providing care to those who are ill and injured.
Accordingly, while the scope of this review was limited,
these multiple failures have generated concerns and perceptions about
the systemic nature of problems related to the delivery of basic
emergency medical services citywide. Such failures mandate immediate
action by management to improve employee accountability. Specifically,
we believe that several quality assurance measures may assist in
reducing the risk of a recurrence of the many failures that occurred in
the emergency responses to Mr. Rosenbaum: systematic compliance testing,
comprehensive and timely performance evaluations, and meaningful
administrative action in cases of employee misconduct or incompetence.
The 911 call from Gramercy Street was received in the
Office of Unified Communications (Communications), which responds to
emergency and non-emergency calls in the District. Communications
centralizes the coordination and management of public safety
communication systems and resources. It is a consolidation of emergency
911, non-emergency 311, and 727-1000 calls for the MPD, FEMS, and
District government customer service operations.
Communications employs an automated system, I-Tracker,
that continuously tracks the location of all mobile emergency units and
identifies the closest unit that can be dispatched to an emergency event. It is Communications
policy to dispatch the closest appropriate unit to the scene of an
emergency.
Documentation provided by Communications management shows
that all universal call takers and dispatchers have the training
required for their positions. This includes training in basic anatomy,
systems of the body, management of different types of calls and callers,
and emergency medical dispatch procedures. Communications management
stated that the national standard for call takers and dispatchers does
not require them to be Emergency Medical Technicians (EMTs).
Based on the answers elicited from a 911 caller,
predicated on a predetermined set of questions asked by the call taker,
an automated system6 categorizes and assigns a priority
designation7 to
each call. Dispatchers then use computer software to identify and
dispatch the closest available units. Radio operators give directions to
locations and provide other assistance as needed. The Director of
Communications stated that the system in place is one of the most widely
used and accepted by the emergency medical community.
According to the Fire and Emergency Medical Services
Department (FEMS) website, FEMS “provides fire protection and medical
attention to residents and visitors in the District of Columbia.” Fire
stations have engine companies and/or truck companies,8 and may have one
or more ambulances. Two paramedics9 are generally assigned to
Advanced Life Support (ALS) ambulances,10 although they
may be staffed by a paramedic and an EMT.11 Two EMTs are assigned to
Basic Life Support (BLS) ambulances. The District has 8 engine companies
with EMTs, 3 heavy-duty rescue squads with EMTs, 19 Paramedic ALS
ambulances, a Rapid Response, 24-hour ALS ambulance, and 17 BLS
ambulances.
When a call comes into a firehouse, a lighted sign alerts
the crew that they are being dispatched to an address, the reason for
the dispatch, and what other emergency responders are being dispatched
to the same call. BLS fire engines are stocked with oxygen, cervical
collars, and a “jump bag.” The jump bag contains plastic airways,
nonrebreather oxygen masks,12 nasal
cannulas,13 bandages, an obstetrical
kit, and vital signs testing equipment. There are no blankets,
stretchers, back boards, or medications on BLS fire engines. Upon
completion of any call, firefighters record minimal details such as
date, time, location, and nature of the call in a log book that is
maintained at the firehouse.
The FEMS Training Division in southwest Washington, D.C.
is responsible for training firefighters. Since 1989, all firefighters
have been required to obtain certification as EMTs. All recruits attend
the training academy for an 18-week course, 6 weeks of which are devoted
to EMT training. EMT candidates who are not firefighters are trained at
private EMT training institutions. In addition to formal training, all
EMT trainees must pass an EMT Basic Certification written and practical
skills examination. This one-day examination is administered by the D.C.
Department of Health, Office of Emergency Health Medical Services
Administration. A score of 75% is required to obtain certification as an
EMT. EMTs must obtain recertification every 2 years by attending a
40-hour refresher course and passing a practical and a written test. In
addition, all firefighters and EMTs must have CPR certification, which
is renewed after refresher training every 2 years.
The National Highway Transportation Safety Administration
(NHTSA), under the federal Department of Transportation, sets standards
and establishes guidelines and curricula for the nation’s emergency
medical services providers. According to NHTSA, there are three levels
of EMT certification: EMT-Basic, EMT-Intermediate, and EMTParamedic. In
2000, pursuant to Special Order 2005-17, FEMS instituted a protocol
course for “EMT-Advanced,” a local program that is intended to
“ensure the highest possibility of care.” The EMT-Advanced program
is not sanctioned by NHTSA. All EMTs were scheduled to attend the
additional protocol course, which included 2 weeks of didactic,
laboratory, and clinical training. Upon completion of all components of
the training, an EMT-Advanced could provide additional pre-hospital
services, such as administering certain medications and performing advanced
airway management. Nonfirefighter EMTs were trained first, and two
classes of firefighter/EMTs were trained in 2002. After 2002, however,
funding for continued training was no longer available, and EMT-Advanced
training ended. EMT-Advanced personnel are given a wallet card with the
EMT-Advanced designation. The card does not expire and EMT-Advanced
refresher training is not required.
FEMS protocols governing medical treatment are based on
NHTSA guidelines, state protocols, U.S. Department of Transportation
training curricula, EMT guidelines, and other reference materials.14 In
addition, FEMS publishes General Orders which dictate operational
procedures for all FEMS personnel. Special Orders update General Orders,
while Memoranda and Bulletins inform personnel of special issues or
changes of note. All FEMS personnel can access the General Orders,
Special Orders, and Memoranda online, and hard copies are kept in
binders at each firehouse. The current FEMS D.C. Adult Pre-Hospital
State Medical Protocols were approved in May 2002, partially revised in
2004, and “apply to every EMS agency that operates in the District of
Columbia.”
FEMS General Patient Care Protocols: EMT-Basic Scope of
Practice, at A-5.1 through A-5.2, outlines what certified EMTs are
authorized to do: evaluate the ill and injured; render basic life
support, rescue, and first aid; obtain diagnostic signs (e.g.,
temperature, blood pressure, pulse and respiration, level of
consciousness, and pupil status); perform CPR; use airway breathing
aids; use stretchers and body immobilization devices; provide initial
pre-hospital emergency trauma care; perform basic field triage; perform
blood glucose testing;15 initiate IV lines for
saline;16 administer
oxygen, glucose, and charcoal; administer selected medications;17 assist
EMT-Intermediates and EMTParamedics; manage patients within their scope
of practice; and transport patients.
The protocol for “Patient Care” states that after
assuring the EMT’s and the patient’s safety, and employing
precautions to prevent contact with body fluids, the EMT performs an
initial assessment “on every patient to form a general impression of
needs and priorities.” According to this patient care protocol, the
initial assessment includes an evaluation of:
- mental status18
- airway
- breathing
- circulation
- disability, which includes
performance of neurological assessment and injuries. This includes removal of clothing as necessary
and maintenance of spinal immobilization, if needed.
This section of the protocol includes a detailed chart
that addresses the “Appropriate Focused History and Physical
Examination” for the unresponsive and responsive patient, which
includes the detailed examination and ongoing assessment that is to be
performed. Upon completion of the assessment, the protocol requires that
a clinical priority be assigned as follows: Priority 1 is Unstable;
Priority 2 is Potentially Unstable; and Priority 3 is Stable.
A “Note Well”19 in the patient care protocol states:
“The provider with the highest level of pre-hospital training and
seniority will be in charge of patient care.”
The Metropolitan Police Department (MPD) is the primary
law enforcement agency for the District of Columbia. General Orders
establish policies and procedures for MPD officers.
MPD General Order SPT-401.01, entitled “Field Reporting
System,” dated March 4, 2004, states, in part, at page 3:
It shall be the responsibility of the first member on the
scene, regardless of his/her assignment, to begin conducting the
preliminary investigation after safety precautions have been taken and
the investigation does not interfere with the criminal case or defeat
the ends of justice.
The General Order “Procedural Guidelines” section
provides on pages 3-4:
The preliminary investigation is the combination of those
actions that should be carried out, as soon as possible, after the first
responding member arrives on the scene. At a minimum, he/she shall:
- Ensure that injured or sick persons receive medical
attention.
- Secure the crime scene to prevent the evidence from being
lost or contaminated.
- Determine whether a crime has been committed and, if
so, the exact nature of the offense or incident.
- Determine the identity of the suspect and make an apprehension when appropriate.
- Provide lookout information to the dispatcher and
other units, such as descriptions, method and direction of travel,
whether armed or unarmed, and any other identifiable information about
any suspect(s) and/or the suspect’s vehicle.
- Identify, interview, and take statements from all
victims, witnesses and suspects to determine in detail the exact
circumstances of the offense or incident.
- Arrange for the collection of evidence.
- Take any other action that may aid in resolving the
situation or solving the crime as directed by a supervisor.
The “Procedural Guidelines” section of this same
General Order further states that the preliminary investigation begins
when the first MPD Officer arrives on the scene of “a crime or
incident.” All information obtained is to be documented on appropriate
forms and submitted for review and signature. The section entitled
“Regulations” states that appropriate reports and paperwork are to
be completed for “[a]ny incident or crime that results in a member
being dispatched or assigned to calls for service.”
Howard University Hospital (Howard) is a 482-bed
university and teaching hospital. Its services include a Level I trauma
center and emergency department that responds to more that 48,000 visits
a year.
An Assistant Clinical Manager oversees all activities of
the Emergency Department, and a Charge Nurse supervises and directs the
patient care activities. One triage nurse is assigned to the ambulance
receiving area known as the “back triage,” and another triage nurse
is assigned to the “front triage” or “walk in” area, where all
patients seeking emergency care,20 are received. In addition, there also
is a “fast track” section for patients who need treatment for acute,
minor illnesses, such as earache, or minor lacerations not needing
sutures. Fast track care is available from 10 a.m. until 12 midnight.
The Emergency Department is organized into two teams:
“Red” and “Blue.” The Red Team works out of the rooms on
hallways “A” and “B,” and the Blue Team works out of the rooms
on hallways “C” and “D.” The teams function separately, with a
team leader and assigned staff nurses. Each team should be staffed with
three Registered Nurses and an “Emergency Department tech.” On
January 6, 2006, there were three registered nurses on the Red Team, two
on the Blue Team, and neither team had an assigned technician.
According to page 1 of the Howard Emergency Department
triage policy, “Triage is designed to provide timely assessment and
management of all patients” who arrive at the Emergency Department.
When a patient enters the Emergency Department, a triage nurse evaluates the patient, performs an assessment, and
indicates what level of care he or she needs. Levels of care are
described in the triage policy. For example, Level I patients have
“conditions which are critical and life-threatening, and which require
immediate therapeutic intervention ….” Level I conditions include
cardiac arrest, unconsciousness, or emergency child birth. According to
Howard’s policy, Level II patients have conditions which are critical
and require immediate intervention after triage. These conditions
include cardiac chest pain, sudden headache, and alcohol and drug
intoxication. Level III patients are defined as having conditions which
are not critical or life-threatening, but require immediate intervention
after triage and registration. Howard’s triage policy provides that
patients requiring Level III care, including those with abdominal pain
and victims of child abuse and sexual assault, should be seen within 2
hours. Level IV patients have conditions such as minor burns, dental
injuries, and allergic reactions, for which intervention can be delayed.
The Howard Policy for Admission, dated January 2005,
states that the triage nurse “will utilize the algorithms21 in
determining the priority level of care appropriate to manage the
patient.” According to the algorithm for alcohol abuse, found in the
Howard Emergency Department Triage Manual, a patient with any of the
following is considered a Level II patient:
- abnormal vital signs
- altered mental state (including
combative, loud, inappropriate behavior)
- non-ambulatory
- history of fall or syncope22
- history of acute seizure episode.
A patient with these symptoms goes to the main Emergency
Department, where the staff is to “urgently proceed.” If none of the
above signs are present, the patient is a Level IV.
According to the Office of the Chief Medical Examiner
home page on the D.C. government website, the Chief Medical Examiner:
Investigates and certifies all deaths in the District of
Columbia that occur as the result of violence (injury) as well as those
that occur unexpectedly, without medical attention, in custody, or pose
a threat to public health.
At approximately 9:20 p.m. on January 6, 2006, a resident
of Gramercy Street, N.W. (Neighbor 1) observed an unknown man lying on
the sidewalk directly in front of his house. According to Neighbor 1, he
approached the man, who was lying face up on the ground, and saw that he
appeared to be ill or injured. He was unable to rise. When Neighbor 1
spoke to the man, he responded with groans. Neighbor 1 called to his
wife, Neighbor 2, and told her to dial 911 for assistance. Neighbor 2
relayed the 911 call taker’s questions about the man to her husband.
She then relayed her husband’s answers to the 911 call taker. After
ending the call, Neighbor 2 went outside to see if she could help the
man. According to Neighbor 2, the man was “dressed nicely and not
unkempt.” Stereo headphones were lying next to him, and as he kept
raising his left arm, she noticed that he was wearing a watch and a
wedding band.
Neighbor 2 stated that the man’s eyes did not connect
with hers when she spoke to him, and he did not appear to understand
what was being said to him. He was using only the left side of his body,
as he kept trying to sit up. However, he would fall back each time,
striking his head on the ground. He appeared unable to use his right
side, and was never able to sit up or stand up. Neighbor 2 also stated
that her husband, who was wearing slippers, placed his foot under the
man’s head to keep it from hitting the ground. Neighbor 2 brought a
blanket from the house and covered the man, and she and her husband
knelt on either side of him while waiting for the ambulance. Neighbor 1
stated that he did not notice any bleeding, physical harm, or trauma to
the patient’s body from the time he found him until he was transported
to the hospital. However, after the man was put into the ambulance,
Neighbor 1 did notice a wet spot on the ground where the man had been
lying. He stated that he could not tell what it was until the next
morning, when he recognized it as blood.
According to Communications records and recordings, the
911 call from Neighbor 2 was answered by a call taker at 9:27 p.m. The
call taker interviewed Neighbor 2 by using software-generated questions
to assess the nature of the problem. According to the call taker, after
she keyed in the answers provided by Neighbor 2, the software made an
assessment of the call and produced a description of “Unknown Problem
(man down).” The software also determined that a dual response by FEMS
and MPD was warranted. This information was transmitted electronically
to both the FEMS and MPD dispatchers.
In July 2005, FEMS issued a policy change entitled
“Revised Dispatch Policy Change # 3.” The purpose of the policy
change was “to improve ALS and BLS response times by dispatching ALS
units on Charlie and Delta Level responses and BLS units on Alpha and
Bravo Level responses.” According to this policy, “Bravo Level calls
will be handled by a first responder and a Basic Life Support Unit. ALS
units will no longer be dispatched on Alpha or Bravo Level calls.” The
policy further states that if the first responders (firefighter/EMTs) on
the scene request an ALS unit, they must notify Communications with an
update on the patient’s condition, and the requested ALS unit will be
dispatched. The Gramercy Street call was classified as requiring a
“Bravo” level (BLS) response from FEMS.
Using the information elicited by the call taker, the
software identified, selected, and recommended as first responders,
Engine 20, and BLS Ambulance 18. The Communications Event Chronology23
indicated that Engine 20 was .54 miles, and Ambulance 18 was 5.61 miles
from the Gramercy Street incident. At 9:30 p.m., the FEMS dispatcher
radioed Engine 20, located at 1617 U Street N.W., and Ambulance 18,
which was at Providence Hospital (Providence) on Varnum Street, N.E., to
respond to the Gramercy Street incident.
According to the Event Chronology, at 9:31 p.m., MPD unit
2022 was dispatched to respond to the Gramercy Street call.
Communications software had designated the call a Priority 2, and
required the dispatcher to relay this information to a police unit
within 10 minutes. At 9:37 p.m., MPD unit 2021 with Officer 1 and
Officer 2, contacted Communications and advised that they would take the
Gramercy Street call, and that MPD unit 2022 should disregard that call.
MPD unit 2022 driven by Officer 3 acknowledged this message, but advised that she would
respond to the location and would “remain in service.”
Communications staff followed
protocols. Based on the Office of the Inspector General’s (OIG) review
of Office of Unified Communications’ protocols, procedures, tape
recordings, and employee interviews, the OIG team determined that the
call taker and dispatchers who handled the Gramercy Street 911 call
carried out their duties appropriately. According to Neighbor 2, when
she made the 911 call, the call taker was thorough, helpful, and
courteous. Further, the team’s review of the taped 911 call shows that
the call taker worked according to the predetermined script, and sent
the call information to the FEMS and MPD dispatchers within the allotted
time of 60 seconds.
None.
On January 6, 2006, at 9:30 p.m., Communications
dispatched Battalion 4, Engine 20, headquartered at 1617 U Street, N.W.,
to the Gramercy Street 911 call. According to interviews and the Event
Chronology, Engine 20, a BLS vehicle, arrived on the scene at 9:35 p.m.
Four firefighters responded to the Gramercy Street 911
call: FF, FF/EMT 1, FF/EMT 2, and FF/EMT 3. A review of FEMS personnel
records showed that three of the four, FF/EMT 1, FF/EMT 2, and FF/EMT 3
had current EMT certifications.24 FF/EMT 2 was an EMT-Advanced. FF, who
was the officer in charge that evening, had never been trained or
certified as an EMT.
FF has been a firefighter at Engine Company 20 for 24
years. When he was hired, EMT training was not required. After such
training became a requirement, FF still never received training.
According to FF, he “just fell through the cracks.” FF informed his
supervisor about his lack of training but was never put into a class.
The last time FF tried to get into a class was 6 years ago. FF’s CPR
certification expired 2 years ago, and he does not have first aid
training.
On January 6, FF’s immediate supervisor was sick, and
he was designated as the “acting officer in charge,” supervising the
activities of the crew assigned to Engine Company 20. FF was assigned to
this supervisory position even though he was not trained, certified, or
in any way qualified to oversee the firefighter/EMTs’ care and
treatment of ill or injured persons.
According to FF, Engine Company 20 personnel received a
call for a “man down” on Gramercy Street, N.W. around 8:30 or 9 p.m.25 They responded and found a man lying on the sidewalk. The
firefighter/EMTs began attending to the patient. The patient immediately
began to vomit, and the firefighter/EMTs had to clean him up with gauze
pads retrieved from the jump bag. The vomit smelled like alcohol. “It
was like food, not a lot of vomit. It kind of dribbled down his
jacket.” When asked who put gauze to the back of the patient’s head,26 FF initially stated, “[FF/EMT 2] or [FF/EMT 1].” Later in
the interview, FF stated, “I don’t remember anyone placing gauze on
the patient’s head. We used gauze to clean up the vomit.”
FF radioed dispatch to ask for status of the responding
ambulance and was told that Ambulance 18 was responding from Providence.
He could tell by the radio traffic that it was pretty busy that night
and that only a few ambulances were available.
FF spoke with the couple who had called 911. Neighbor 1
said he was going out to his car when he saw the patient. FF/EMT 1
started a patient assessment to check for injuries, and Neighbors 1 and
2 placed a blanket on the patient. FF/EMT 1 was holding the patient in
the sitting position with FF/EMT 1’s legs supporting the patient’s
back.
FF/EMT 3 took the first set of vital signs, and FF/EMT 2
the second. FF “watched them do this because [he] wanted to make sure
[his] guys were doing the right things.” The firefighter/EMTs wore
gloves, and he saw them “feel for trauma and blood. They found no
signs of trauma or blood.” The patient vomited at least two more
times. FF stated that the patient “never spoke, but was conscious and
a little combative when we tried to place oxygen on him.”
The lighting in the area where the firefighter/EMTs were
working was dim. FF’s recollection was that he turned the truck light
on to provide more illumination. FF stated that a female police officer
arrived and stayed in the car. Soon after, other MPD officers arrived.
After Engine 20 firefighter/EMTs had “taken the
patient’s vitals and stabilized him, all the ambulance had to do was
pull the stretcher out and take the patient to the hospital.” When the
ambulance arrived, FF talked with a female EMT, who asked, “What do we
have?” One of the firefighters replied by telling her, “ETOH.”27
The male EMT never inquired about the patient. Either FF/EMT
2 or FF/EMT 3 gave the female EMT the patient’s vital signs, which had
been written on a firefighter/EMT’s glove. FF did not see her write
them down. The male EMT placed the patient into the back of the
ambulance, and the female EMT sat in the driver’s seat. FF asked where
they were going and the female EMT stated, “Howard.”
When asked about the firefighters’ EMT training and the
level of pre-hospital care they could provide, FF stated that no one was
an EMT-Advanced.28 He knew this because their nametags would show their
status.
Subsequent to the Gramercy Street call, FF wrote a report
as directed by FEMS officials, and submitted it to his battalion chief.
On January 18, an interview panel comprised of FEMS and Department of
Health officials at Company 20 firehouse interviewed him about the
Gramercy Street call.
FF/EMT 1 has been a firefighter/EMT since May 1992. He
was recertified as an EMT-Basic in the fall of 2004. FF/EMT 1 is based
with Engine Company 9, but on January 6, he was detailed to Engine
Company 20 to help staff a shift that was shorthanded. FF/EMT 1 stated
that Engine 20’s regular driver, FF, was the acting officer in charge
that night.
FF/EMT 1 recalled that when Engine 20 arrived at the
Gramercy Street address, “two or three, but not more than four, people
were standing right over” a man lying on the sidewalk. The man was on
his back, moving and moaning. He described the man’s movement as
“squirming,” and remembered that the patient must have vomited
because he saw vomit on him. FF/EMT 1 stated that he did not smell
alcohol at that time.
According to FF/EMT 1, he helped FF/EMT 2 and FF/EMT 3
take the patient’s left arm out of his jacket so that someone could
take his blood pressure. They sat the patient up and took turns holding
him in a sitting position because he was vomiting. FF/EMT 1 recalled
that the patient vomited at least twice while Engine 20 was there. FF/EMT
1 stated that he checked for a medical identification (ID) bracelet, but
he did not find one. He stated that he usually performs this kind of
check, “especially when people can’t talk.” FF/EMT 1 remembered
hearing one of his colleagues announce that he was going through the
patient’s pockets looking for identification, but could not remember
who said it. FF/EMT 1 explained that firefighter/EMTs say this out loud
to avoid the perception by observers that they are searching patients’
pockets in order to steal their belongings.
FF/EMT 1 put an oxygen mask to the patient’s face and
“cranked it up,” meaning that he was giving the patient 15 liters of
oxygen per minute in order to “get him to come around.” When asked
if the patient was unconscious, FF/EMT 1 responded, “He was moaning,
and he couldn’t respond. I didn’t know what was wrong.” The
patient repeatedly took the oxygen mask off, and FF/EMT 1 kept putting
it back on. FF/EMT 1 stated that he did not know who took over the
oxygen mask duty when he left the patient’s side, but there were three
firefighter/EMTs and, “We were all doing everything. We all switched
up.” He stated that he could not describe what the other firefighter/EMTs
did for the patient because he was concentrating on giving the patient
the oxygen, which “was hard enough.” FF/EMT 1 could not say whether
other firefighter/EMTs gave the patient medications, performed an
assessment, provided any other care, or determined the cause of the
patient’s illness.
When FF/EMT 1 was asked what firefighter/EMTs are
required to do when they arrive at an emergency, he stated, “all we
are supposed to do is take vital signs and stabilize until transport
comes.” When asked what stabilizing efforts might be made for a “man
down,” FF/EMT 1 replied, “There’s a long list of stuff we could
do. I don’t know.” He then said that firefighter/EMTs could do
“everything except push drugs.” FF/EMT 1 also stated that
firefighter/EMTs could radio to Communications and inform the call
center that a call is of a more or less serious nature than originally
dispatched. FF/EMT 1 did not describe any medical urgency related to the
patient’s condition. In addition, since the man had no medical alert
bracelet identifying him as a diabetic, the firefighter/EMTs did not
consider him to be a diabetic.
FF/EMT 1 went to the truck and turned on the sidelights.
The position of the truck and its lights did not make the illumination
“real bright,” but it was better than without them. FF/EMT 1
returned to the patient and continued giving oxygen. At some point, two
MPD officers arrived, but FF/EMT 1 did not know them, nor was he able to
describe what they said or did. FF/EMT 1 remembered that
the night was cold, and he heard other firefighters ask for a blanket,
which a citizen provided. The firefighter/EMTs used the blanket to cover
the patient. The patient was shaking his head and vomiting, which made
the vomit “go everywhere.” FF/EMT 1 could smell alcohol, but he
thinks it was the vomit.
After the ambulance arrived, the ambulance crew did not
ask FF/EMT 1 any questions, and he did not talk to them. He overheard
others talking to them, but was not paying attention to what was being
said. FF/EMT 1 helped one of the ambulance EMTs put the patient on the
ambulance cot and move the patient into the ambulance.
Engine 20 returned to the firehouse, and FF/EMT 1
completed his shift at 7 a.m. on January 7. FF/EMT 1 did not make a
written report on January 6 on the care provided to the patient but
noted that “generally,” the firefighter/EMT who assesses the patient
writes notes and vital signs “on the glove or whatever” and gives
the glove to the ambulance personnel.
When FF/EMT 1 returned to work on January 10, there was
an order that he write a special report regarding the Gramercy Street
call. FF/EMT 1 wrote the report, and submitted it to his battalion
chief. He stated that an interview panel at Company 20 firehouse
interviewed him about the Gramercy Street call.
FF/EMT 2 has been a firefighter/EMT with FEMS for almost
4 years and has been at Engine Company 20 for the last 1½ years. Both
his CPR and EMT certifications are current. FF/EMT 2 has received EMT-Advanced
training.
FF/EMT 2 recalled that on January 6 the regular engine
driver, FF, was the acting officer in charge. FF/EMT 2 was the engine
driver for the night. When Engine Company 20 personnel arrived at the
Gramercy Street address, they saw a person lying on the sidewalk.
According to FF/EMT 2, the driver usually does not leave the truck.
However, he could see that the patient was vomiting, and because he had
the highest level of training, he left the truck to assist his
colleagues.
One of the firefighter/EMTs performed a sternum rub29
when they first arrived, and FF/EMT 2 gave the patient oxygen via a non-rebreather
mask. However, the patient vomited again. FF/EMT 2 removed the oxygen
mask so the patient could vomit freely. After FF/EMT 2 removed the
oxygen mask, he smelled alcohol. FF/EMT 2 recalled that when FF/EMT 1
put the oxygen mask back on the patient’s face, the patient “kind of
grimaced and pushed the oxygen mask away from his face.” FF/EMT 2
described the patient as “in and out of it,” but the oxygen
“brought him around. The patient was compliant, but didn’t like the
oxygen. If I tapped him he would look around at me.”
When MPD officers arrived on the scene, FF/EMT 2 asked
them if he could check the patient for identification. FF/EMT 2 went
through the patient’s pockets, but did not find anything.
FF/EMT 2 stated that he performed a patient assessment,
took the patient’s vital signs, and checked the patient’s head. His
assessment consisted of palpating30 the patient’s head, upper back,
neck, lower back, and the front of his chest. He found a speck of blood
on the patient’s head above his right ear. There was no swelling, and
there were no lacerations. FF/EMT 2 applied pressure to the patient’s
head with 4 x 4 gauze pads. This stopped the bleeding, which was
minimal. FF/EMT 2 “checked [the patient’s] motor responses and they
were fine.” FF/EMT 2 wrote the patient’s vital signs on a piece of
paper, which he retrieved from the jump bag, and gave the paper to FF/EMT
3. When he was asked if he always writes the vital signs down, FF/EMT 2
replied, “Yes, this is how it’s done.” Vital signs are recorded
and the writing is provided to the ambulance crew. FF/EMT 3 also took
vital signs as well as at least two additional blood pressure readings.
FF/EMT 2 recorded FF/EMT 3’s readings.
According to FF/EMT 2, FF/EMT 1 performed an assessment
of the patient’s lower body, which included everything below the
patient’s waist. The patient was sitting up with help from FF/EMT 1,
who had the patient’s back against his legs to hold him up. FF/EMT 2
stated that the patient would look at the firefighters but would not
respond when asked a question. FF/EMT 2 stated that the patient wore a
wedding band and a “nice” watch, and there was a one-piece radio
headphone set in the grass nearby.
According to FF/EMT 2, “It was cold that night, so I
got a blanket from the truck and a person that was standing there, a
female neighbor, placed a nice blanket on the patient. I remember
hearing someone say, ‘Get the blanket; get the blanket,’ because the
patient was vomiting [on it].” The firefighter/EMTs placed the patient
on the neighbor’s blanket to get him off the ground, and placed the
firefighters’ blanket on top of him.
When asked if he checked the patient’s pupils, FF/EMT 2
replied, “Yes, with my Streamlight.”31 According to FF/EMT 2, the
pupils were constricted, meaning small and not reacting to light.
Because the interviewers recognized this as a symptom requiring further
assessment, they asked if he was sure of the pupil response. FF/EMT 2
then changed his statement and said the patient’s pupils did react,
and they “contracted,” meaning they became smaller when exposed to
light.
The ambulance arrived, and the female EMT asked the
firefighters, “What we got?” FF/EMT 3 told her, “ETOH.” FF/EMT 1
and FF/EMT 3 helped the Ambulance 18 crew load the stretcher with the
patient onto the ambulance, and care of the patient was transferred to
the EMTs. The patient was not placed on a back board and did not have a
neck collar. Engine 20 returned to the firehouse after clearing trash
from the scene.
FF/EMT 2 wrote a report and submitted it to his battalion
chief. FF/EMT 2 stated that an interview panel at Engine Company 20
firehouse interviewed him about the Gramercy Street incident.
FF/EMT 3 has been a FEMS firefighter for 15 years. He has
worked at Engine Company 20 for 4 years. FF/EMT 3 remembered they
received a call at the firehouse on January 6 to Gramercy Street for a
“man down.” Engine 20 arrived on the scene and FF/EMT 3 went to the
side of the truck to retrieve supplies. The other firefighters went to
the patient. While he was retrieving supplies, a woman approached and
told him she had found the man on the ground.
The patient was vomiting by the time FF/EMT 3 got to him.
FF/EMT 3 repositioned the patient’s head so he would not choke. The
vomit looked like a full meal and was red. FF/EMT 3 then assessed the
patient’s level of consciousness. He stated that the patient:
was looking at me sarcastically. He never said anything.
I could smell the alcohol reeking from him, like it was coming out of
his pores. I tried talking with him, but he didn’t speak. I told him
we were going to take his blood pressure, but he was not really
complying.
FF/EMT 3 took one of the man’s arms out of his coat in
order to take his blood pressure.
Because the patient did not tell them what was wrong,
they performed a head-totoe assessment. After checking the patient, FF/EMT
3 saw a speck of what he thought was blood on his white gloves. He
checked the patient again but could not find where the speck came from.
He stated he thought it was food from the vomit.
Firefighter/EMTs tried to give the patient oxygen at 25
liters per minute, but the patient took the oxygen mask off. FF/EMT 3
stated that the patient “kept rolling his eyes at me.” FF/EMT 3
stated that the patient was not combative and was “okay after I turned
down the oxygen. He let the oxygen mask stay on a lot longer.” The
only thing notable about the patient’s condition was that he did not
respond verbally or follow commands.
FF/EMT 3 stated that when MPD units arrived, there were
two black male officers and “one black lady [officer] in her vehicle,
chillin’.” FF/EMT 3 told one officer standing nearby that he was
going to go through the man’s pockets for ID but could not find any.
FF/EMT 3 stated, “Just from growing up, I thought something was wrong.
I found it odd that the patient did not have a wallet or ID on him. No
one usually walks around with nothing. I told the guys, ‘Somebody got
him,’ meaning he was robbed.” His colleagues said, “Yeah,
something’s wrong.” The MPD officer just shrugged.
FF/EMT 3 stated that he took one set of vital signs,
which he explained included “pulse, respiration, and blood
pressure.” FF/EMT 2 took vital signs two more times.
FF/EMT 3 stated that he “took the lead, but mostly I
had [FF/EMT 2] doing most of the stuff. Even though [FF/EMT 2] is a
higher level by training, because he’s an EMTAdvanced, I always take
the lead because I have more time on [the job].” The patient’s vital
signs were stable, and FF/EMT 2 wrote them on the back of his glove. FF/EMT
3 stated, “I never write down vitals. How hard is it to remember them?
I give it to them [the ambulance crew] orally.” FF/EMT 2 told him that
the patient’s pupils were “pinpoint,”32 meaning, according to FF/EMT
3, “small.” According to FF/EMT 3, FF/EMT 2 did not give him
anything in writing.
The ambulance arrived, and FF talked to the female EMT. A
male EMT put the patient into the back of the ambulance. FF/EMT 3 gave
an oral briefing to the male EMT on the patient’s vital signs.
FF/EMT 3 wrote a report and submitted it to his battalion
chief. An interview panel at Engine Company 20 firehouse interviewed him
about the Gramercy Street incident.
Neighbors 1 and 2 told the OIG team that while the
arrival time of the fire truck was good, they believed the ambulance
took too long to get there. When the firefighter/EMTs arrived, Neighbor
2 asked them if they would be able to help and “kept trying to talk to
them,” but they did not pay any attention to her. Neighbor 2 thought
the injured man had a stroke. She believes that she heard the
firefighters rule out a stroke or heart attack. Neighbor 1 heard the
firefighters say that “9 out of 10 times it’s alcoholrelated.”
Neighbors 1 and 2 did not smell alcohol on the patient’s breath.
Neighbor 2 saw the firefighter/EMTs give the patient
oxygen, and that seemed to make him vomit. She saw him vomit twice. The
firefighter/EMTs wiped the vomit from his mouth with what looked like a
“Kleenex.” They kept trying to sit him up, and at the same time,
they were “tapping on his chest.” According to Neighbor 2, the
firefighter/EMTs did not appear to know what they were doing. She
explained that they were not cohesive and were just standing around not
doing anything specific other than giving the patient oxygen and waiting
for the ambulance.
- Firefighter had no CPR
certification. FEMS protocol requires that all fire personnel have
current CPR certification. FF advised that his CPR certification has not
been current for 2 years. Despite his expired CPR certification and the fact that he was not an EMT, FF was
in charge of the crew. He also stated that he monitored their actions to
ensure that they performed correctly.
- EMT with highest level of
pre-hospital training not in charge. The firefighter/EMT with the
highest level of pre-hospital training, FF/EMT 2, did not take charge of
patient care during the Gramercy Street call as required by protocol.
- Oxygen delivery contrary to
protocol. FF/EMT 3 administered oxygen to the patient at 25 liters per
minute (LPM). This action exceeded both FEMS protocol33 and accepted
medical practice of 15 LPM.
- Perceived alcohol intoxication
dictated firefighter/EMT actions. Firefighter/EMTs could not obtain a
health history or a cogent response from the patient. They stated that
they smelled alcohol, and assumed that the patient’s altered mental
status was solely caused by intoxication. Firefighter/EMTs did not
consider that in addition to having consumed alcohol, the patient could
be experiencing other illnesses or conditions such as stroke, drug
interaction or overdose, seizure, or diabetes. They also disregarded the
possibility that head trauma or other injury could have contributed to
his altered mental status.
- Spinal cord injury potential
disregarded. FF/EMT 1 described sitting the patient up and removing his
clothing prior to assessing him for head, spinal, or other injuries
which would have made moving the patient from a prone position
inadvisable. FF/EMT 3 described moving the patient’s head prior to
assessing his level of consciousness or the presence and extent of
injury. In addition, firefighter/EMTs described their continuing efforts
to keep the patient in an upright position, despite the patient’s
inability to sit up, which is an indication of possible head or spinal
cord injury.
- Diabetes discounted due to absence
of medical ID bracelet. Firefighter/EMTs made assumptions about the
patient’s medical condition because of the absence of a medical ID
bracelet. FF/EMT 1 stated that the absence of a medical ID bracelet for
diabetes eliminated their concern that diabetes was the cause of the
Gramercy Street patient’s current condition.
- No patient priority assigned.
Firefighter/EMTs did not perform a neurological assessment of the
patient, and did not assign the patient a priority as required by the FEMS Patient Care Protocol. This
protocol is described in the “Operations and Protocol” section of
this report.
- Faulty patient assessment. No single
firefighter/EMT performed a complete patient assessment, which resulted
in a patient assessment that was disjointed and incomplete. According to
the firefighter/EMTs, they divided the patient’s body in half. One
assessed the lower body, while the other assesed the top half. Two took
the patient’s blood pressure a total of four times, two took vital
signs, two gave oxygen, and one checked the patient’s pupils. None of
the vital signs was recorded, and only one set was communicated verbally
to the male EMT.
- Suspicion of criminal attack not
followed-up. When firefighter/EMTs checked for the patient’s ID, they
noted that he did not have a wallet or any ID on his person. FF/EMT 3
relayed to the OIG team that he said out loud, in the presence of his
colleagues and an MPD officer, that he thought the patient had been
robbed. However, even though his FEMS colleagues agreed that something
was “wrong,” neither FF/EMT 3 nor the other firefighter/EMTs
conducted a thorough assessment of the patient for assault-related
injuries or communicated this concern to the EMT who assumed care of the
patient. FF/EMT 3 also did not connect his stated suspicion to the
physical signs he observed. These indicators included vomiting,
combativeness, bleeding, and non-responsiveness, all of which are
symptoms indicative of a head injury.34
- Inadequate assessment performed
after blood found. Firefighters/EMTs FF/EMT 2 and FF/EMT 3 described
finding blood when they examined the patient. Neither reported using the
available flashlight to inspect the patient’s head and body for the
source of the blood.
- No follow-up to critical finding
regarding pupils. FF/EMT 2 told FF/EMT 3 that the patient’s pupils
were “pinpoint,” meaning that the pupils were constricted and
unresponsive. FF/EMT 3 stated that he, FF/EMT 3, had seniority and
always “took the lead.” Both firefighter/EMTs should have known that
pinpoint pupils are abnormal and warrant follow-up. However, neither
conducted any follow-up, nor did they connect the condition to other
symptoms the patient displayed. In addition, neither FF/EMT 2 nor FF/EMT
3 conveyed this information to Ambulance 18 EMTs.
- Scope of EMT practice misunderstood.
FF/EMT 1 gave an incomplete description of firefighter/EMTs’
responsibilities as “taking vitals and stabilizing the patient until
transport arrives.” In addition, FF/EMT 1 incorrectly described the
scope of EMT practice as “EMTs can do everything except push drugs.”
FEMS protocols clearly describe the EMT scope of practice, which is summarized in the “Operations and
Protocols” section of this report.
- Oral communication flawed.
Firefighter/EMTs at the scene conveyed minimal information to the
Ambulance 18 EMTs upon their arrival. Although FF/EMT 2 and FF/EMT 3
noted seeing blood when they examined the patient, they did not relay
this information to Ambulance 18 EMTs. FF/EMT 2 told FF/EMT 3 that the
patient’s pupils were constricted; however, neither FF/EMT 2 nor FF/EMT
3 relayed this information to the EMTs. FF/EMT 3 stated that he thought
the patient had been robbed, but did not convey his suspicion to
Ambulance 18 EMTs. According to the firefighter/EMT statements, vital
signs were assessed multiple times; yet the male EMT stated that he only
received one set of vital signs verbally from FF/EMT 3. FF/EMT 3 told
the male EMT that the patient was “just intoxicated.”
- FEMS requirement for written report
not followed. There was no written patient care report prepared on
January 6 by any firefighter or firefighter/EMT who responded to the
Gramercy Street incident. However, FEMS Special Order Number 49, “Fire
Fighting Division Units on Medical Locals,” dated September 6, 1996,
requires taking the patient’s vital signs, including but “not
limited to pulse, respiration, pupil response, skin color, skin
temperature, and blood pressure,” and recording them on Form 902 EMS.
The OIG team was told that Form 902 EMS has not been used for some time
because it is undergoing revision. Some information about the Gramercy
Street incident was logged in the Engine Company 20 firehouse journal.
- The OIG team reviewed the firehouse log book for entries
prior to and subsequent to January 6, 2006 in order to determine the
type of information routinely documented. Medical-related calls were
documented with minimal detail. However, the January 6 entry made for
the Gramercy Street call appears to contain information that was added
to the original entry. Similar information is not present in any entries
on dates prior to January 6, or on subsequent dates reviewed by the OIG
team. The additional information included a blood pressure and pulse
reading, and the word “verbal” written in a different color ink from
the original entry. The added entries also included the notation: “MPD
on scene.” Finally, it appears that a sentence was changed with an
overwritten word.
- Contradictory interview statements about documenting
patient information. Although three firefighters made statements
indicating that care information was documented, their statements were
inconsistent and confusing. FF stated that either FF/EMT 2 or FF/EMT 3
wrote the vital signs on a glove and gave it to the Ambulance 18 female EMT. FF/EMT 2 stated that he
wrote his own and FF/EMT 3’s vital sign readings on a piece of paper
retrieved from the fire truck “jump bag,” and that he gave the paper
to FF/EMT 3. FF/EMT 3 stated that FF/EMT 2 wrote the vital signs on the
back of his glove. FF/EMT 3 also stated that he gave an oral briefing to
the Ambulance 18 male EMT, and that he got nothing in writing from FF/EMT
2. Ambulance 18 EMTs denied receiving any documentation on a glove or on
paper.
- That FEMS ensure all personnel have current required
training and certifications prior to going on duty. The OIG team
determined that FF, who was in charge of the Engine 20 EMTs responding
to the Rosenbaum call, had not been trained as an EMT, and his CPR
certification had not been current for 2 years.
- That FEMS develop a form that is mandated for use by
firefighter/EMTs who respond to any medical call. First responders’
actions and patient medical information must be documented as required
by Special Order Number 49. The form implemented by FEMS should
identify: 1) the EMT responders; 2) their actions regarding assessments
and pre-hospital medical care; 3) patient information, including
identification, past medical history, chief complaint, current
condition; and 4) other pertinent information. This form would remain
with the patient when care is transferred to other pre-hospital care
givers and Emergency Department personnel.
- That FEMS develop and implement a standardized
performance evaluation system for all firefighters. The OIG team
determined that FEMS firefighters are not evaluated on a regular basis,
in the manner that most other District government employees are
evaluated. According to a senior FEMS official and confirmed by the
District’s Office of Personnel, firefighters have no performance
measures and do not receive written performance evaluations. Grade and
step salary increases occur irrespective of the quality of their work.
Consequently, FEMS lacks standards to guide firefighters’ performance
and for use in evaluating their performance.
- That FEMS assign quality assurance responsibilities to
the employee with the most advanced training on each emergency medical
call. This report documents numerous failures to follow FEMS protocols
that provide guidance for all aspects of the duties performed during
emergency incidents. The OIG team recommends that the senior responder
on each emergency call:
- have in-depth knowledge of the most current protocols,
General Orders, Special Orders, and other management and medical
guidance that govern emergency response activities;
- monitor compliance with FEMS protocols by all personnel
at the scene, and provide on-the-spot guidance to ensure that all key
duties are performed; and
- include the results of on-scene compliance monitoring
in reports as required by FEMS management.
According to the “Event Unit Information,”35 the MPD
dispatcher at Communications dispatched unit 2022 at 9:31 p.m. to the
Gramercy Street scene. Another unit, 2021, which covers the same
geographical area, was finishing a call nearby. Unit 2021 officers
radioed Dispatch at 9:37 p.m. to advise that they would take the
Gramercy Street call because Field Training Officer, Officer 1, wanted
his trainee partner, Officer 2, to gain experience. Officer 1 told
Dispatch that unit 2022 should disregard the call. The “disregard”
communication was radioed to the officer in unit 2022, Officer 3.
Officer 3 acknowledged receipt of the dispatch to disregard the call.
However, she told the dispatcher that she was going to the scene anyway,
and arrived at 9:38 p.m., prior to Officer 1 and 2’s arrival.
Officer 3 has been a police officer at the Second
District for 4 years. She works the “third watch,” which is 2:30
p.m. to 11:00 p.m. During the interview with the OIG team, Officer 3
referred to a written document to help her remember details about the
Gramercy Street incident.
On January 6, Officer 3 received a call for service at
9:30 p.m. for a “man down” on Gramercy Street. She stated that she
did not remember why she went to a scene to which she had been
dispatched and then told to “disregard.” She stated, “It was my
area.”
According to Officer 3, Officers 1 and 2 arrived before
she did.37 She saw firefighters on the scene, and a man sitting upright.
He was “going in and out of consciousness,” and fighting the
firefighters off. One of the firefighter/EMTs told her the man had a
seizure. They also told her that he “appeared drunk.” It looked as
though the firefighter/EMTs put something “small” under his nose,
and every time they did, “he would come around.” Officer 3 asked the
firefighter/EMTs if the man had identification or could give his name
and was told, “No.” Officer 3 stated that she interviewed the male
neighbor whose wife had called 911. She did not try to question the man
receiving treatment. Officer 3 also did not search the man’s clothing
for identification and did not conduct any search or other interview.
The patient tried to stand up, but the firefighter/EMTs
held him down. Officer 3 noted a “patch” on the man’s head, and
that he was vomiting. She did not see an oxygen mask but noted that the
man wore a watch and a ring. Officer 3 remembered that it was dark, and she had her patrol car spotlight on. Officer 3
could not remember if the fire truck had lights on.
Officer 3 left approximately 1 minute after the ambulance
arrived, but she did not notify Dispatch of her departure. When asked if
she wrote a report on the Gramercy Street incident, Officer 3 responded
that she does not write reports when she is not the primary responder.
Officer 1 has been a police officer for 2½ years and has
been at the Second District for 2 years. Officer 1 remembered the
Gramercy Street incident as a call for a “man down.” When he and his
partner in unit 2021 heard the call, they radioed Dispatch to say they
would take it, and to cancel the dispatch of MPD unit 2022. Officer 1
was a field training officer to his partner Officer 2, and wanted
Officer 2 to get experience, so he volunteered to take the call.
When Officer 1 and Officer 2 arrived at the scene, FEMS
Engine 20 was present. Officer 1 stated that Officer 3 was interviewing
a man, presumably the complainant. Officer 1 looked around the scene but
did not immediately talk to the firefighters from Engine 20.
Officer 1 observed a man sitting on the ground vomiting.
According to Officer 1, the man was conscious, his eyes were open, and
he was moaning. Firefighter/EMTs were clearing his mouth and throat.
They were also giving him oxygen and were holding gauze to the back of
his head. Firefighter/EMTs were talking to the man, but he did not
respond to them. Officer 1 did not talk to the man.
Officer 1 talked to the firefighter/EMTs, who said they
were treating the patient for an injury to the back of his head,
possibly caused by a fall or a seizure. Officer 1 was not close enough
to smell alcohol and did not look for the man’s ID. The man being
treated looked like a “regular person” who belonged in the area. He
was “not out of place.” The man was wearing jewelry and stereo
headphones were on the ground nearby. Officer 1 did not collect the
headphones as possible evidence.
Officer 1 stated that he and Officer 2 talked to the male
complainant (Neighbor 1) and asked if he knew the man or knew how he got
there. The complainant responded that he did not know the man or what
happened to him. When the ambulance arrived, the man was placed on a
stretcher and moved into the ambulance. Officer 1 did not talk to the
ambulance EMTs. He remembered a white male EMT, but he did not remember
anything about the other EMT. When asked if he wrote a report following
the incident, Officer 1 stated, “No, not for a drunk.” He stated
that reports concerning drunks are completed by FEMS.
Officer 2 has been a police officer for a year. He
attended the MPD training academy from January–September 2005 and has
been at the Second District since then. Officer 2 works the third watch.
On January 6, he was in training and was partnered with Officer 1, who
was his Field Training Officer.
Officer 2 remembered the Gramercy Street incident. When
he and his partner heard the call for a “man down,” they radioed
Dispatch to say they would take it and to cancel the other unit. When
they arrived at the scene, Officer 3 and the firefighters were there.
Officer 2 saw a man sitting on the ground who was not talking.
Firefighter/EMTs were holding something white, either a towel or a
bandage, to the back of his head. Officer 2 saw a quarter-sized spot of
blood on the bandage. He asked the firefighter/ EMTs what was wrong, and
one told him the man was “possibly intoxicated. He fell and hit his
head.” Officer 2 does not know which of the firefighter/EMTs said
this. He asked where the ambulance was coming from, and a firefighter/EMT
told him the ambulance was coming from Providence Hospital. Officer 2
asked why it was coming from Providence, and was told that it was the
closest one.
Officer 2 “did not get a close look at the man,” and
saw “no signs of an assault.” He saw that the man had on a watch and
a wedding ring but did not search for ID or talk to the man. Officer 2
asked a firefighter/EMT if the man had any ID and was told he did not.
Officer 2 stated that he talked to “the complainant,”
who said that he did not know the man lying in front of his residence
and did not know how he got there. Officer 2 wrote identifying
information on the complainant in his notebook.
Officer 2 stated that the ambulance arrived, staffed by a
male and female EMT. Firefighter/EMTs and the male EMT put the patient
into the rear of the ambulance. Officer 2 asked the male EMT where they
were going with the patient, and he stated, “Sibley.” The female EMT
then said, “No, we’re going to Howard.” He stated that he thought
it was curious that they were going to Howard because they were closer
to other hospitals.
Officer 2 stated that he gave statements regarding the
Gramercy Street call to his captain, the MPD Violent Crimes Branch, and
to the United States Attorney’s Office. He had a copy of the report
that he wrote for the internal investigation conducted in the MPD Second
District regarding the MPD response and provided a copy to the OIG team.
While working overtime following his regular shift,
Officer 1 heard a radio call concerning a missing person and responded
to the caller’s home. After being shown a photograph of the missing
person, David E. Rosenbaum, Officer 1 recognized the man in the
photograph as the same individual in the “man down” call on Gramercy
Street who was transported to Howard by Ambulance 18. Officer 1 relayed
this information to MPD officials, who subsequently verified that Mr.
Rosenbaum was a patient at Howard.
On Saturday, January 7, Mr. Rosenbaum’s daughter
notified MPD that several credit card companies had contacted her
father’s residence regarding suspicious activity on her father’s accounts. This information, combined
with MPD’s knowledge that Mr. Rosenbaum was a patient at Howard,
prompted notification to the MPD Violent Crimes Branch, which assumed
investigative responsibility for the case, and opened an assault and
robbery investigation.
- No search of the “man down” for
identification. MPD General Orders require that a preliminary
investigation shall include identification of “victims, witnesses and
suspects.” The three responding MPD officers stated that they did not
search the man for identification. Instead, the officers relied on the
firefighter/EMTs’ search for identification, which was conducted in
the course of carrying out emergency medical activities. Two
firefighter/EMTs stated that they searched the patient for
identification.
- No preliminary investigation.
Officer 3, the first MPD officer to arrive at the Gramercy Street scene,
did not conduct a preliminary investigation, secure the scene, or
determine if a crime had been committed. Officer 3’s failure to
perform these steps violated MPD General Orders as described in the
“Operations and Protocols” section of this OIG report. No
explanation was provided as to why this officer responded to a call that
she had been told to disregard, why she did not consider herself to be
the first responding officer, and why she did not conduct a preliminary
investigation. The two officers who assumed the primary responsibility
for the call, Officers 1 and 2, also failed to conduct a preliminary
investigation, secure the scene, and determine if a crime had been
committed.
- No connection made between the
man’s condition and possible crime. MPD officers stated that they
found a semi-conscious individual who could not speak or give
information about his identity, residence, or circumstances. The
officers stated that they observed a bandage or gauze being held to the
back of the man’s head, and one officer said that he saw blood on the
bandage. The man was wearing a watch and ring, stereo headphones were
lying on the ground nearby, but he had no wallet or identification.
Despite these facts, the officers did not connect the man’s condition
with the possibility that a crime had been committed.
- No report on incident completed. MPD
officers did not complete a report pursuant to the General Order
SPT-401.01 “Field Reporting System,” Section IV A, which states,
“[m]embers shall investigate and complete the appropriate reports38
and paperwork as outlined in this General Order in the following situations … [a]ny incident or crime that results in a
member being dispatched or assigned to calls for service.” The
officers responsible for investigating the subsequent missing person
report made by Mr. Rosenbaum’s wife had no information about the
“man down” on Gramercy Street incident that occurred just 2 hours
earlier, not far from the Rosenbaum residence. It was merely by
coincidence that Officer 1 was on overtime duty and recognized the
subject of the missing person report as the man found on Gramercy
Street.
That MPD immediately review and reissue the pertinent
General Orders relating to officer responsibilities at emergency
incidents. In addition, MPD should consider implementing or revising as
necessary a quality assurance program that includes supervisory review
of required reports, and a tracking system to ensure that reports are
written and retrievable for every call.
That MPD assign quality assurance responsibilities to
the senior officer responding to each call. This officer would:
have in-depth knowledge of the most
current General Orders, Special Orders, and other management guidance
that governs emergency response activities;
monitor compliance with MPD General
Orders and other guidance by all personnel at the scene to ensure that
all key actions are taken; and
include the results of on-scene
compliance monitoring in reports as required by MPD management.
According to Communications Event Unit Information, BLS
Ambulance 18 with an EMT-Advanced and a firefighter/EMT-Basic was
dispatched at 9:30 p.m. and arrived at Gramercy Street at 9:53 p.m.
Ambulances are designed to transport patients from the scene of an
emergency to a medical facility. Minimum staffing consists of two
certified Basic EMTs. Ambulances cannot exceed the speed limit and must
stop for all red lights. The vehicle is equipped with a Direct Entry
Keyboard (DEK) system, which enables the ambulance crew to communicate
electronically with Communications regarding the vehicle’s location
and status. Its purpose is to provide “real time” response time
calculations and to reduce radio traffic between emergency responders
and Communications. Ambulance crews use the DEK system to indicate that
they have received a message, have arrived on a scene, are available for
service, are in transport, or have arrived at a hospital. Ambulance
medical equipment includes a cot (stretcher), backboard and cervical
collars, splints, bandaging supplies, oxygen, and an automatic
defibrillator.
The two EMTs responding to the Gramercy Street call on
January 6 were EMT 1 and EMT 2. As an EMT-Advanced with the highest
level of pre-hospital training, EMT 1 was “Ambulance Crewmember in
Charge” (ACIC), and EMT 2 was “Ambulance Crewmember Assistant.”
According to a review of FEMS files, both EMT 1 and EMT 2 have current
EMT certifications.
EMT 139 has worked for FEMS since 2001. Prior to that,
she was a dispatcher for MPD for a year. EMT 1 received EMT training at
a private emergency medical technician training program. EMT 1 renewed
her EMT certification in July 2005. According to EMT 1, she was
qualified as an EMT-Advanced, but that “certification expired 2 years
ago.” EMT 1 stated that she has not renewed it, or pursued the
necessary retraining to regain certification as an EMT-Advanced.
However, the OIG team reviewed a document written and signed by EMT 1 in
August 2005 on which she indicated that her status was “EMT-A[dvanced].”
In addition, the OIG team reviewed documents written in November and
December 2005 in which EMT 1 is referred to as an “EMT-Advanced.”
EMT 1 has worked at Engine Company 18, Ambulance 18,
quartered at 414 8th Street, S.E., for the past 2 years. Three EMTs,
including EMT 1, are assigned to that firehouse, and two of the three
have partners. EMT 1 has no partner, so she works with a different
firefighter/EMT on every shift depending on the firehouse work schedule.
EMT 1 said she had worked with EMT 2 many times, and EMT 2 thinks she is
an EMTAdvanced. EMT 1 and EMT 2 alternate driving and patient care
duties.
On January 6, EMT 1 reported to work at 7 p.m. As the
ACIC, she was responsible for checking the equipment and stocking the
ambulance. EMT 1 considered herself to be the ACIC because, according to
her, it is a “seniority kind of thing,” based on time on the job. As
ACIC, EMT 1 could determine the patient priority level and override her
partner’s decisions.
EMT 1 remembered that on January 6, they were at
Providence Hospital around 9:30 p.m when the Gramercy Street call came
in. EMT 1 was outside smoking and believes that she answered the call.
EMT 1 indicated that she “knew where to go as soon as [Communications]
said ‘3800 block of Wisconsin.’ I have never been to Gramercy but I
have been to that area.” The OIG team played the dispatch call tape
for EMT 1 on which a male voice could be heard answering Dispatch and
asking for directions. After listening to the tape, EMT 1 stated, “I
thought I answered the call, but I can’t remember everything.”
When asked if she protested going to Gramercy Street, EMT
1 denied protesting. The OIG team then played the tape, on which EMT 1
is heard questioning why Ambulance 18 was being sent to Gramercy Street.
On the tape, the dispatcher tells EMT 1, “The lead [dispatcher] says
you are to go to this call. If another unit closer becomes available, it
will be sent there.” The OIG team then asked EMT 1 if it is usual for
an EMT to question Dispatch about being sent on a particular call, as
EMT 1 had done on the tape. EMT 1 replied, “That’s my right. I can
question anything. They ain’t always right.”
EMT 1 described how she and EMT 2 left Providence Hospital.40 EMT 1 stated that “her partner” was giving her
directions, and they drove to Rhode Island Avenue, to Florida Avenue,
and to Connecticut Avenue. She did not recall the exact route from
Connecticut Avenue to Gramercy Street.
When they arrived at the Gramercy Street scene, EMT 1 saw
four to five firefighters, and a patient sitting or lying on the
sidewalk in front of a house where there was a man on the porch. It was
a cold, clear night. The patient on the sidewalk “was a white male,
conscious and breathing with vomit all over him.” According to EMT 1,
the man had a lot of vomit on his shirt and jacket. EMT 1 assumed he was
a drunk because he had vomit all over him. The patient never said
anything to her. She did not get close enough to smell alcohol because,
in her words, “It wasn’t my patient.”
According to EMT 1, firefighter/EMTs usually give the
ambulance crewmembers some information or “a little story” about the
patient. However, this time they provided no story or information. EMT 1
asked Engine 20 personnel, “What we got?” They replied, “ETOH.”
EMT 1 responded that she replied, “We came all this way for an ETOH?”
EMT 1 does not remember which of the firefighter/EMTs said what.
According to EMT 1, none was wearing gloves, no one said anything other
than “ETOH,” and no medical information was given. A male
MPD officer was present, but did not say anything.
EMT 1 did not assess the patient. EMT 2 and a firefighter
put the patient on a stretcher, and she helped them put the stretcher on
Ambulance 18. EMT 1 asked EMT 2, “You okay?” EMT 2 replied, “I got
it.” Before driving away, EMT 1 waited for EMT 2 to finish his
assessment of the patient. EMT 2 told her the patient was a “[Level]
3.”41 EMT 1 radioed Communications that she had a “[Level] 3 to 5
[Howard].” When asked if she questioned EMT 2 about the patient’s
priority level, EMT 1 replied that she did not argue with her partner
regarding the patient’s status. EMT 1 stated, “If he said it was a
3, it was a 3.”
The OIG team asked why they did not take the patient to
Sibley Hospital. EMT 1 stated, “We can go where we want to go.
[Howard] was available, and he was deemed a low priority.” When asked
if she wanted to go to Howard, EMT 1 initially said “No,” then
changed her answer to “Yes” and said she knew the way to Howard from
Gramercy Street.
At Howard, EMT 1 and EMT 2 unloaded the patient, and EMT
2 took the patient’s vital signs. EMT 1 went outside to smoke. When
she returned, the nursing staff told her and EMT 2 to put the patient in
a bed “around the corner.” The OIG team asked EMT 1 how long
Ambulance 18 was at Howard. EMT 1 could not remember exactly but said,
“It was a while.” EMT 1 said that she cleaned up the ambulance.
There was not a lot of vomit, just some that appeared to have come from
the sleeve of the patient’s jacket. EMT 1 did not smell alcohol or
vomit in the ambulance.
When asked what Ambulance 18 did after leaving Howard,
EMT 1 initially stated that they went to back to the firehouse. EMT 1
then stated that she thought that she drove the ambulance to her house
to get money for dinner and then went to the firehouse on 8th Street,
S.E.
After returning to the firehouse, Ambulance 18 was taken
out of service. In the early morning hours of January 7, EMT 1 was sent
home on administrative leave. EMT 1 stated that she had never been sent
home before, did not know why she was sent home, and could not remember
who sent her home. She thinks a lieutenant made the decision. She asked
the lieutenant why she was being sent home, and why her partner, EMT 2,
was reassigned to a fire truck. EMT 1 called the firehouse 2 hours
later, and was told about statements from the FEMS Medical Director that
the Gramercy Street patient should have been a Level 1.
EMT 1 had to write a special report, which she submitted
to a lieutenant, whose name she could not remember. On January 18, 2006,
a FEMS interview panel interviewed EMT 1 about the Gramercy Street call.
The team reviewed the FEMS interview panel’s January 24, 2006, report
regarding the Gramercy Street incident and found multiple discrepancies
between EMT 1’s statements to the interview panel and those made to
the OIG team.
On Monday, January 10, EMT 1 was told to go to Engine
Company 16 at 1018 13th Street, N.W. for retraining. At the time of her
OIG interview, EMT 1 stated that she was in a training unit and, upon
completion of retraining, would be assigned to an ambulance. EMT 1
stated that the retraining included 2 days of classroom training and
occasional ambulance calls. According to EMT 1, she “[was] not
learning anything.”
EMT 2 is a firefighter/EMT who has worked for FEMS for 5
years. He previously worked as an EMT in Colorado for 5 years. He is
assigned to Battalion 2, Engine Company 18, located at 414 8th Street,
S.E. EMT 2 is assigned to ambulance duty approximately once or twice per
month.
EMT 2 has worked with EMT 1 many times. He always works
with her because, at this firehouse, she is the only civilian
(non-firefighter) EMT who does not have a permanent partner. EMT 2
stated that all civilian EMTs are EMT-Advanced level. According to EMT
2, when an EMT-Advanced and an EMT-Basic are working together, the
EMT-Advanced is in charge of patient care. Some teams split the driving
and patient care duties, but if the patient in the back of the ambulance
is “bad off,” the EMTAdvanced needs to be with the patient. EMT 2
described an EMT-Advanced as a “Basic EMT with a broader scope of
practice,” such as starting IVs and administering drugs with a
doctor’s orders.
According to EMT 2, both EMTs are responsible for
checking the ambulance and stocking it prior to departure, although the
previous crew should ensure that it is ready. Both he and EMT 1 checked
the ambulance on January 6. EMT 2 checked the treatment area, and EMT 1
checked the cab. EMT 2 stated that there is a map of the District in the
cab of the ambulance. EMT 1 announced at the beginning of the shift that
she was going to drive. EMT 2 stated that EMT 1 likes to drive during
the first half of the shift and provide patient care during the second
half.
EMT 2 stated that the first call of the night ended at
Providence Hospital, which was “not that busy.” After dropping the
patient at Providence, EMT 1 told EMT 2 that she wanted to go to the ATM
near their firehouse at 8th and Pennsylvania Avenue, S.E. to get money
for dinner. EMT 2 and EMT 1 were outside of the hospital smoking when he
heard radio traffic asking for the status of three or four different
ambulance units. EMT 2 pushed the button on the DEK to notify
Communications that Ambulance 18 was available for a call. He also
radioed Communications via the ambulance radio that they were available.
EMT 2 stated that EMT 1 became agitated because he had put them back
into service. She yelled at him, “Don’t touch the radio!”—
meaning that he was not to answer the radio calls.
According to the Communications Event Unit Information
for the Gramercy Street call, Communications dispatched Ambulance 18 to
Gramercy Street, N.W. at 9:30 p.m., and put it “en route” at 9:31
p.m.44 EMT 2 stated that EMT 1 did not want to go to upper northwest.
They pulled out of the Providence Hospital area with EMT 1 driving. EMT
1 advised EMT 2 that she did not know where Gramercy Street was and told
him to get directions. Meanwhile, EMT 1 was driving toward Rhode Island
Avenue, which is in the opposite direction from their intended
destination.45 EMT 2 told EMT 1 to stop and pull over, but she refused.
According to EMT 2, “She was gonna do what she was gonna do.”
Ambulance 18 advised Communications via the DEK that they
were en route to Gramercy Street at 9:40 p.m. EMT 2 asked Dispatch for
information about the location. He could not understand the dispatcher
because of her accent, and asked for clarification. Dispatch advised
that Gramercy was off Wisconsin, Harrison, and Garrison. EMT 2 told EMT
1 that he needed the map. EMT 1, who stated during her OIG interview
that she had checked and stocked the front of the ambulance prior to
departure, told EMT 2 that she did not know where the map was. EMT 2
found it behind his seat.
By the time EMT 2 figured out where Gramercy Street was,
using the directions from Dispatch and the map, Ambulance 18 was at the
intersection of Rhode Island and Florida Avenues. EMT 2 stated that it
took Ambulance 18 about 20 minutes to get to Gramercy Street from that
location.
While Ambulance 18 was en route to Gramercy Street, EMT 1
told EMT 2 that she wanted to go to Howard because she had a toothache
and wanted to go to her house for medicine. EMT 1 then wanted to get
some money from a nearby ATM for dinner. EMT 1 complained to EMT 2,
“This is b*******. We shouldn’t be all the way up here.”
According to the Event Unit Information, Ambulance 18
arrived at Gramercy Street at 9:53 p.m. EMT 2 saw Engine 20 personnel
with a patient who was sitting up. One firefighter/EMT was standing
behind him, holding him up. It was hard to distinguish the
firefighter/EMTs from each other because none of them wore identifiable
D.C. Fire Department uniforms. It was cold and they were all covered up.
EMT 2 stated that EMT 1 approached one of the responders, who was about
20 feet away from the patient, and started talking to him.
FF/EMT 3 approached EMT 2, who asked FF/EMT 3 what was
going on. FF/EMT 3 told him that the patient was “just intoxicated.”
EMT 2 asked if they needed a collar and board, and FF/EMT 3 repeated,
“No, he’s just intoxicated.” FF/EMT 3 gave EMT 2 one set of vital signs for the patient. EMT 2
stated that he did not receive any written documentation from the
firefighters.
The area was dark, even with the fire truck’s light on.
One MPD officer had a flashlight that he was shining in the area where
the patient lay. The patient was a 60-70 year old white male who was
covered with a blanket. EMT 2 took the blanket off and observed that the
patient had vomit on his face and chest. According to EMT 2, “the
vomit did not smell like anything.” Engine 20 firefighter/EMTs told
EMT 2 that they had tried to give oxygen to the patient but he took the
oxygen mask off. EMT 2 described the patient as incoherent, and
“growling” incomprehensible words. EMT 2 recalled seeing many
citizens standing around the scene, and the police holding them back.
EMT 2 did not assess the patient while he was lying on
the sidewalk because he wanted to get him out of the cold and away from
all the people. EMT 2 stated that it is easier to do assessments inside
the ambulance. The firefighter/EMTs did not relay to him significant
medical information about the patient, such as his bleeding head wound.
In addition, they did not give EMT 2 any written documentation of the
patient’s vital signs.
EMT 2 determined they needed to take the patient to the
hospital. EMT 1 came over to the patient with a yellow blanket from the
ambulance and wrapped the patient in it. Firefighters helped EMT 2 move
the patient onto a cot and move the cot into the ambulance. A MPD
Officer asked what hospital they were going to, and EMT 2 told him they
were going to Sibley Hospital because they were “not that far from
Sibley.” EMT 1, however, said, “No, not Sibley. We are going to
Howard.”
At 9:58 p.m., Ambulance 18 left the Gramercy Street scene
with EMT 1 driving. EMT 2 asked where they were, and EMT 1 told him she
was trying to get back to Connecticut Avenue. EMT 1 told him she did not
know where they were, and it “took a bit” to get to Connecticut
Avenue.46 EMT 2 radioed Communications and told them they were taking
the patient to Howard as a Level 3.
EMT 2 took the patient’s pulse and blood pressure and
recorded them on the 151 Run Sheet.47 EMT 2 tried to put the oxygen mask
on the patient, but the patient took it off. EMT 2 performed a Glasgow
Coma Scale (GCS)48 assessment. He stated that the GCS is a way to
measure a patient’s level of consciousness. He assessed the patient as
having a low GCS, which he stated meant that something was wrong.
The patient started vomiting, so EMT 2 moved the
stretcher into an upright position. EMT 2 checked the patient’s head
and checked his pupils by using his thumb and forefinger to open the patient’s eyelids, letting
the overhead ambulance light shine in his eyes. The pupils were
reactive. EMT 2 did not document the pupil test results. He did not
undress the patient, but checked the patient’s legs, pelvis, and
abdomen by palpating those areas through his clothing.
EMT 2 stated that it took 20 minutes for Ambulance 18 to
get to Howard. According to the Event Unit Information, Ambulance 18
arrived at Howard at 10:18 p.m. As Ambulance 18 was pulling into the
hospital, EMT 2 took the patient’s vital signs and performed a second
GCS assessment, which was the same as his first assessment. He noticed
that the patient’s blood pressure had fallen.
EMT 2 told the triage nurse the patient was intoxicated.
The triage nurse took the patient’s blood pressure and walked away.
When she returned, she told EMT 2 and EMT 1 to put him in the hallway.
EMT 1 and EMT 2 moved the patient onto a hospital stretcher in the
hallway.
EMT 1 went outside to smoke, and EMT 2 went into a room
in the Emergency Department to document the patient’s pre-hospital
care on the 151 Run Sheet. EMT 2 then took the 151 Run Sheet back to the
nursing area and asked a nurse to sign it. The nurse who signed the 151
Run Sheet as the “Person Receiving Patient,” was not the triage
nurse who received the patient on his arrival. EMT 2 left a copy of the
151 Run Sheet with the nurse who signed it. EMT 2 acknowledged to the
OIG team that the 151 Run Sheet was not filled out completely, which was
a violation of FEMS protocol.
EMT 2 stated that he cleaned Ambulance 18 prior to
leaving Howard.
Ambulance 18 left Howard with EMT 1 driving. EMT 1 drove
to Massachusetts Avenue, N.W., where one of her children brought
medication from an apartment to the ambulance. According to EMT 2, EMT 1
told him the medication was Tylenol 3 for her toothache. EMT 1 intended
to go to an ATM, but Ambulance 18 was dispatched to a call in the
Trinidad area of the city. After completing the Trinidad call, Ambulance
18 returned to the firehouse at 8th and Pennsylvania Avenue, S.E.
Shortly after arriving at the firehouse, telephone calls
started coming in about the Gramercy Street incident. EMT 2 and EMT 1
were told the patient’s condition had worsened, and Ambulance 18 was
taken out of service. EMT 2 was reassigned to a fire truck and finished
his shift. EMT 2’s supervisor told EMT 2 and EMT 1 that they had to
prepare special reports on the Gramercy Street incident. Subsequently,
EMT 2 had to appear before the FEMS interview panel to answer questions.
EMT 2 stated that FEMS Acting Medical Director required
that he and EMT 1 go to the FEMS Fire Academy for 2 days of classroom
and skills training on altered mental status and proper completion of
paperwork. They were the only two people in the class. The retraining
included instruction on assessment for altered mental status, the
Glasgow Coma Scale, head trauma, and proper documentation. EMT 2
received a FEMS protocol manual for the first time since he had been
employed at FEMS.
- Highest-trained EMT not in charge of
patient. General Patient Care Protocols: Patient Care, states at page
A1.5, “[t]he provider with the highest level of pre-hospital training
and seniority will be in charge of patient care.” On Ambulance 18, EMT
1, who was an EMT-Advanced, had the highest level of pre-hospital
training. In addition, both EMT 2 and EMT 1 considered her to be the
Ambulance Crewmember in Charge. However, EMT 1 delegated patient care
duties and responsibilities to EMT 2, an EMT-Basic. It is unclear to the
OIG team why an EMT-Advanced working with an EMT-Basic would not
consider herself responsible for anything other than driving the
ambulance. In fact, EMT 1 made a point of distancing herself from the
care of the Gramercy Street patient. She told OIG interviewers
explicitly that, “It wasn’t my patient.” She neither assessed the
patient herself, nor helped her partner assess him. When
firefighter/EMTs offered very little information about the patient,
other than his presumed intoxication, she failed to question them about
the patient’s vital signs or other aspects of his condition. EMT 1
also failed to inquire about the care and treatment they had provided.
EMT 1 told the OIG team that she assumed the patient was a drunk because
he was covered in vomit.
- Glasgow Coma Scale assessment result
disregarded. General Patient Care Protocols: Adult & Pediatric
Clinical Priority and Transport Decision Chart identifies a patient with
a GCS assessment of less than 13 as unstable. EMT 2 assessed the
patient’s GCS twice: once after departing Gramercy Street en route to
Howard and again as the ambulance was arriving at the hospital. The
first reading was described by EMT 2 as low and meaning that something
was wrong. The second reading was the same as the first. However,
neither EMT increased the patient’s priority, or informed Howard
Emergency Department personnel about the low GCS scores.
- Incorrect clinical priority
assigned. The General Patient Care Protocol: Patient Care, “Initial
Assessment” section requires that after the EMT conducts an initial
assessment, he or she must assign a clinical priority. The “Adult and
Pediatric Clinical Priority and Transportation Decision Chart”
protocol sets forth a list of conditions for each clinical priority. For
example, Priority 1 Medical49 includes patients with cardiac arrest, GCS
of less than 13, and multiple trauma. The Gramercy Street patient’s
GCS was less than 13, but he was incorrectly categorized as a stable
patient, or Priority 3.
- Failure to comply with extended
on-scene service policy. An August 24, 2005, FEMS memorandum, “Chute
Times and On Scene Times,” states that “[a]ll providers are
responsible for assessing, treating, transporting, and returning to
service in an expedient manner.” The memorandum goes on to provide
that “any foreseen extended on-scene time that may be greater than 20
minutes” requires the unit to notify a supervisor and document the
cause of the extended time. According to the Event Unit Information
record, Ambulance 18 arrived at Howard at 10:18 p.m. A photocopy of the
151 Run Sheet shows the ambulance as back in service at “23:26”
(11:26 p.m.), indicating that Ambulance 18 was out of service for more
than 1 hour without notifying a supervisor or documenting the cause of
the extended time on the scene. However, the original 151 Run Sheet is
blank in the area for “InService” time.
- Confusion about the route to
Gramercy Street prolonged the trip. The ambulance crew left Providence
Hospital prior to obtaining adequate directions to the Gramercy Street
emergency. EMT 1, the self-designated driver, got lost after being
dispatched from Providence Hospital at 9:30 p.m. She and EMT 2 were
confused about the route, could not immediately locate the ambulance
map, started driving in a direction that was the opposite of their
intended destination, and had to contact Communications for assistance.
- In addition, Ambulance 18 did not take a direct route
from Providence Hospital, located at 1150 Varnum Street, N.E., to the
Gramercy Street, N.W. address. This trip is approximately 5.67 miles,
with an estimated driving time of 17 minutes.50 I-Tracker indicated that
Ambulance 18 took a route from Providence to Gramercy Street which,
according to MapQuest, added 1.59 miles and 6 minutes to the trip.
According to the Event Unit Information, Ambulance 18, which was using
flashing lights and sirens, arrived at Gramercy Street at 9:53 p.m., 23
minutes after dispatch.
- Discrepancy regarding Ambulance
18’s en route time. There is an unexplained 10-minute gap between the
time Ambulance 18 was dispatched at 9:30 p.m. to Gramercy Street, and
the time EMT 1 engaged the DEK at 9:40 p.m. to show that they were en
route.
- Confusion about the route to Howard
prolonged the trip. According to MapQuest, the trip from Gramercy Street
to Howard is an estimated 4.81 miles, with an estimated driving time of
15 minutes. According to I-Tracker, EMT 1 drove Ambulance 18 from
Gramercy Street in the opposite direction from their destination. Consequently, Ambulance 18
arrived at Howard 20 minutes after leaving Gramercy Street.
- A thorough patient assessment was
not conducted. General Patient Care Protocols direct a comprehensive
initial assessment of every patient “to form a general impression of
needs and priorities.” EMT 1, who had the highest level of
pre-hospital training and was the senior crew member, did not take
charge of patient care as required by FEMS protocols. Although EMT 2
stated that he conducted some of the required assessments, he did not
document all of them on the 151 Run Sheet. Some of the assessments that
were not performed included a capillary refill test,51 assessing the
patient for injuries with his clothing removed, pulse oximetry,52 and a
blood glucose test. The pulse oximetry and blood glucose tests would
indicate if the patient’s inability to speak was related to oxygen
deprivation or a diabetes-related condition. As an EMT-Advanced, EMT 1
was trained to perform the blood glucose test and should have done so
prior to Ambulance 18’s departure for Howard.
- Pupil check not properly performed.
Based on his own statement, EMT 2 did not conduct a proper pupil check.
He stated that he used his thumb and forefinger to let the overhead
ambulance light shine in the patient’s eyes rather than using a
penlight or other focused light source.
- Patient’s clothing not removed for
a thorough examination. General Patient Care Protocols state, “[t]o
assess the patient’s injuries, remove clothing as necessary,
considering condition and environment.” EMT 2 stated that he did not
want to assess the patient on the sidewalk because of the cold weather.
However, when the patient was moved into the ambulance, EMT 2 did not
remove any of the patient’s clothing in order to examine his body for
possible injuries.
In summary, the patient could not speak, did not respond
to oxygen delivery, had vomited several times, had a dangerously low GCS
as well as an elevated pulse rate. All of these assessed clinical signs
were indicators of a more serious condition than “ETOH,” which the
EMT wrote on the 151 Run Sheet and communicated to the Howard Emergency
Department staff.
- The transport decision was not based
on FEMS Protocol. The FEMS protocol for “Adult Medical Emergencies:
Altered Mental Status (NonTraumatic)” requires that EMTs
“[t]ransport patient to the closest appropriate open facility.”
Sibley Hospital was the closest appropriate open hospital from Gramercy
Street.53 The decision to transport Mr. Rosenbaum to Howard rather than
Sibley, however, was not based on his medical needs or an assessment
that he was a trauma patient who required a trauma center such as
Howard. Mr. Rosenbaum was transported to Howard based on personal
reasons, which delayed the emergency hospital care that would have been
available minutes earlier.
- Although not a trauma center, Sibley Hospital has
emergency and imaging departments that could have provided initial
medical emergency assessment and diagnostic services to Mr. Rosenbaum.
Preliminary medical interventions (e.g., laboratory tests, intravenous
fluids, medications, spinal stabilization, xrays, and a MRI and CT scan)
could have been expeditiously provided in a hospital setting within a
matter of minutes had Mr. Rosenbaum been transported to the nearest
facility, as required by FEMS protocol. We recognize that the discovery
of Mr. Rosenbaum’s head injury may have necessitated his transfer from
Sibley to a facility more appropriate for the trauma care and
neurosurgical intervention he needed.
- EMT 2 told a MPD officer that the patient was being
transported to Sibley, but he was overruled by EMT 1, who said they were
going to Howard. According to EMT 2, before they arrived at the Gramercy
Street incident, EMT 1 had told him twice that she wanted to go to
Howard for personal reasons.
- Ambulance 18 EMTs did not properly
document their actions. A July 1, 2005, Special Order, “EMS 151c Form
Modification,” signed by FEMS Chief Adrian Thompson underscores the
importance of the FEMS 151 Run Sheet. This Special Order states that the
patient-care portion of the form 151 “is a discoverable medical-legal
record, and the primary document pertaining to the care provided any
patient by the Department.” It states further that the form 151’s
contents “are a direct reflection of the Department’s competence,
commitment and professionalism with regards to patient care.”
According to a Patient Care Protocol “Note Well,” the 151 Run
Sheet is not considered complete until it is filled out in its entirety.
However, the 151 Run Sheet completed by EMT 2 was not completely or
properly filled out. For example, he did not document on the first page
of the 151 Run Sheet that he administered oxygen and performed a pupil
response test, although he stated during his interview that he had
carried out these activities. In addition, no times are documented to
show when any treatment, care, or testing was provided or performed.
Finally, the second section of the form related to patient care was left
blank.
- Transfer of patient from FEMS to
Emergency Department Staff faulty. After arriving in the Emergency
Department with the patient, EMT 2 transferred care to the triage nurse
and gave her an oral report on the patient’s condition. He did not
give her the patient’s 151 Run Sheet because it had not been
completed. After completing the 151 Run Sheet, EMT 2 presented it to a
different nurse, who had not seen or assessed the patient and had not
been given a report on the patient’s condition. EMT 2 accepted this
nurse’s signature as the “Person Receiving Patient.”
The OIG team determined that the findings cited above are
attributable to individual failures to adhere to existing policies,
procedures, and protocols during the Gramercy Street incident on January
6, 2006. Consequently, because the OIG team’s focus was on this
singular event, we do not conclude that these failures are necessarily
systemic. They do, however, indicate possible areas of concern related
to management oversight of personnel, accountability for performance,
and quality assurance. Therefore, the OIG team makes the following
recommendations for FEMS management:
- That FEMS ensure all personnel have current required
certifications prior to going on duty. The OIG team determined that EMT
1’s EMT certification expired in May 2005, and she was not recertified
until July 2005. The OIG team reviewed Ambulance 18’s log book at the
Ambulance 18 firehouse and 151 Run Sheets for May to July 2005. The team
found that EMT 1 continued working and providing pre-hospital care
during the period in which she was not certified.54
- That FEMS take steps to comply with its own policy on
evaluating EMTs on a quarterly basis. The OIG team was told that
non-firefighter EMTs have performance measures and are given performance
reviews. However, a battalion fire chief stated that although FEMS
policy requires quarterly EMT evaluations, officials are not meeting
that schedule because “there are too many EMTs to evaluate four times
per year.” Consequently, supervisors evaluate EMTs’ performance
“when time permits,” and some have not been evaluated “in
years.” FEMS officials stated that they are trying to improve their
record on completing performance evaluations, at least annually.
- That FEMS move promptly to reassign, retrain, or
remove poor performers. The OIG team reviewed personnel files of all
FEMS personnel involved in the January 6, 2006, Gramercy Street call.
This review indicated that infractions have been committed by FEMS
personnel for which no disciplinary action was taken. In other
instances, disciplinary action was recommended but not carried out for
several months. While there were disciplinary actions in the files of
firefighters and one EMT for serious infractions, none of these files
involved issues related to pre-hospital patient care.
- That FEMS assign quality assurance responsibilities to
the pre-hospital provider with the most advanced training. This report
documents numerous failures to follow FEMS protocols that provide
guidance for all aspects of the duties performed during emergency
incidents. The OIG team recommends that FEMS consider designating the
most highly-trained responder on each emergency call as the Quality
Assurance Officer, who would be required to:
- have in-depth knowledge of the most
current protocols, General Orders, Special Orders, and other management
and medical guidance that govern emergency response activities;
- monitor compliance with FEMS
protocols by all personnel at the scene, and provide on-the-spot
guidance as necessary; and
- include the results of on-scene
compliance monitoring in those reports already required, and in any
other reports required by management.
Monitoring for quality assurance would not be burdensome
and is already an inherent responsibility of the person in charge. This
recommendation has the potential to provide management with timely
feedback on the quality of the services rendered by individual emergency
responders, as well as a larger picture of the effectiveness of
protocols, policies, and procedures, and any changes that might be
required.
- That FEMS consider installing global positioning
devices in all ambulances to assist EMTs in expeditiously arriving at
destinations in response to emergency calls.
Five Howard Emergency Department nurses and an Emergency
Department physician had responsibility for Mr. Rosenbaum’s care in
the Emergency Department on January 6. All of the nurses are registered
nurses, with current licenses issued by the District of Columbia.
Licenses are renewed every 2 years, with proof of 24 hours of continuing
education during the prior 2-year period.
All of the interviewees emphasized how busy the Emergency
Department was on the evening of January 6, and all stressed that they
were “short staffed.” Optimum staffing is 13, including nurses and
Emergency Department technicians. On January 6, there were 10 staff
members working in the Emergency Department. The doctors and nurses
interviewed stated that all of the rooms were occupied, and patients
were lined up on both sides of the hallways during the period that Mr.
Rosenbaum was a patient.
Nurse 1 has worked at Howard for approximately 5 years.
She works a regular 12-hour shift of 7:30 a.m. to 8:00 p.m., sometimes
working overtime until midnight. On January 6, Nurse 1 worked from 4:00
p.m. to 12:00 a.m. as a triage nurse in Howard’s Emergency Department.
Nurse 1 started the shift working in the walk-in triage
areas. Nurse 1 was told to cover for the nurse at the ambulance triage
area while that nurse went on a break. She described the patient flow in
the Emergency Department, which starts with an assessment by the triage
nurse. If the patient needs treatment in the Emergency Department, the
triage nurse asks the charge nurse to assign the patient to a team. The
charge nurse alternates patient assignments between the teams. If there
is no room available, the patient waits in the waiting area. If the
patient is on a stretcher, the patient is wheeled into one of the
hallways of the assigned team. Once the triage nurse gives information
about a patient to the charge nurse and completes the top portion of the
triage form, “HUH EMERGENCY NURSING DATA BASE M.R.,”5she has no
further responsibility for the patient. The paperwork goes into a chart
rack located in one of the Emergency Department hallways. The chart rack
is divided into sections for the Red and Blue teams. The chart does not
stay with the patient who might be moved to a different location in the
Emergency Department.
Nurse 1 remembered the patient who was brought in by
ambulance. He was signed in at 10:30 p.m. and presented as an
“ETOH,” or intoxicated person. She recalled that a male EMT told her
the patient was drunk and had fallen on the street. Nurse 1 could not
recall if the EMT told her the patient’s vital signs.
Nurse 1 did not see or sign the 151 Run Sheet. She stated
that sometimes EMTs will give the triage nurse a blank 151 Run Sheet and
ask a nurse to sign it. The EMT will then fill in the run sheet before
leaving the hospital.
Nurse 1 recalled that she already had three patients in
the ambulance triage area. The Ambulance 18 patient was one of two
“Does.”60 The stretcher was upright, with the patient in a sitting
position. He was covered with a yellow FEMS blanket. He had no blood on
his face and had a large amount of vomit on his shirt which smelled of
alcohol. He was not talking and looked as if he was asleep. She thought
he had been talking to the FEMS staff and was now asleep, so she “just
let him sleep.”
Nurse 1 recalled performing a triage assessment of the
patient by taking his vital signs, including his oxygen saturation
level, temperature, blood pressure, and heart rate. She took an axillary61 temperature, recognized that the temperature reading was low,
and circled the reading on the triage form. Nurse 1 assumed that “his
temperature was representative of the temperature outside because it was
a cold night.” When Nurse 1 was asked what she did to address the
patient’s low temperature, Nurse 1 stated that she did not retake the
temperature, nor did she use another thermometer or site,62 to ascertain
a second reading. Instead, she stated that she put a Howard hospital
blanket on him.63 Nurse 1 then stated that she circled the temperature
on the triage form so that one of the nurses assigned to his care would
“put a blanket on him.”
According to Nurse 1, the patient was not in respiratory
distress, had no blood on him, and “was not really that sick.” She
did not check his pupils because she “thought he was asleep” and did
not want to bother him. The EMT told her that they had spoken with the
patient earlier, so she indicated that he was “awake and alert,”
even though she did not speak to him, hear him talk, or see any sign
that he was awake or alert. Nurse 1 decided not to wake him because,
according to her, sometimes medical staff has to restrain intoxicated
patients when they wake up and want to leave the Emergency Department.
If the patient’s gait is not steady, medical staff cannot let patients
leave. Nurse 1 did not want this to happen with this patient.
When asked if she considered the patient to be
responsive, Nurse 1 responded, “I saw he was not in distress so I did
not wake him. He just fell asleep so I did not want to wake him.” When
asked how she would know if he was in distress, Nurse 1 stated, “It
would show in his oxygen saturation,”64 which she considered normal.
When questioned further about retaking vital signs because they may
appear inaccurate or alarming, Nurse 1 stated she “never retakes, even
if [she has] reservations about the readings.”
When asked who determines the level of care assigned to a
patient, Nurse 1 stated the level of care is determined at triage before
the charge nurse gets the paperwork. She stated that an intoxicated
patient is usually considered a Level III.65 She determined this patient
was a Level III and circled that designation on the triage form.
Nurse 1 signed the triage form at 10:36 p.m., and then
gave it to the charge nurse, Nurse 2. Nurse 1 told Nurse 2 the patient
was intoxicated and asked where he was to be assigned. Nurse 2 had just
assigned an intoxicated patient to the Red Team, so this patient was
assigned to the Blue Team. Nurse 2 told Nurse 1 to put the patient in
Hallway D.
Nurse 2 has worked at Howard for 17 years, the first 6
years on medical surgical floors, and the past 11 years in the Emergency
Department. She is licensed as a registered nurse in the District of
Columbia and Maryland.
Nurse 2 usually works from 7:30 p.m. to 8:00 a.m. When
she arrived for work at 7:30 p.m. on January 6, she assumed charge nurse
duties from the Assistant Clinical Manager. As charge nurse, Nurse 2
takes reports about patients from the triage nurse, and makes decisions
regarding patient assignments.
Nurse 2 stated that the triage nurse usually gives the
charge nurse the triage form with the top part of the form filled in
with information on the patient. In addition, the charge nurse may get
patient information verbally from the triage nurse. Nurse 1 was assigned
to walk-in triage, but was also covering ambulance triage while the
ambulance triage nurse took a break. Nurse 1 gave Nurse 2 a triage form
on the Ambulance 18 patient. Nurse 2 stated she did not look at the form
in detail. She remembered specifically that he was a “Doe,” and
Nurse 1 saying, “We have another ETOH.” Nurse 2 had just given the
Red Team an ETOH, so this patient went to the Blue Team. Nurse 1 told
Nurse 2 that the patient did not give his name, was not talking, and was
classified as a “Doe.” The EMT from Ambulance 18 also said the man
was intoxicated. Nurse 2 described a man on a stretcher in an upright
position. He was breathing, had vomit on his clothes, was dressed, and
was covered with a yellow FEMS blanket.
Nurse 2 said Nurse 1 did not tell her that the patient
was awake and alert. If Nurse 1 had told her that, she would have
questioned why he was considered a “Doe.” If he had been awake and
alert, he should have been able to give his name. Nurse 2 also stated
that Nurse 1 did not tell her about the patient’s low temperature.
Nurse 2 did not notice the temperature reading on the triage form. She
said if she had known about the low temperature reading, which was
abnormally low, she would have instructed Nurse 1 to retake the
temperature.
Nurse 2 stated that the triage nurse assigns the priority
level, I-IV. Hospital protocol calls for an intoxicated patient to be
considered a Level II patient. In this case, Nurse 1 classified the
patient as a Level III. Nurse 2 would have considered this patient a
Level II and had no explanation for why he was classified as a Level III
in triage.
The bottom of the “Doe’s” form was not completed
with the required assessment information, because the assessments were
not done. The patient became a trauma team patient and the “trauma
flow” sheet was used instead. When asked about the assessment
information required on the form (e.g., GCS, pupil checks, skin
integrity, breath sounds), Nurse 2 stated that it would provide a lot of information
about a patient’s condition if the tests were timely performed. Nurse
2 could not explain why no one had filled in this information, even
though the patient had been in the Emergency Department for some time.
According to Nurse 2, the charge nurse is responsible for
informing the team leader about the patients. The nurse that Nurse 2
thought was the team leader (Nurse 4) was with a trauma patient, so
Nurse 2 could not tell him about the new patient on his team. Nurse 2
stated that the other nurse on the Blue Team, Nurse 3, “knew about the
patient.”
The nurse who is assigned to a patient finds a room,
cleans the patient, performs a finger stick to check for hypoglycemia,
administers oxygen if a person is breathing abnormally, and performs
neuro checks.66 Nurse 2 acknowledged that “no one looked at this
patient.” The Emergency Department was understaffed and very busy.
Nurse 2 stated that a patient waiting 1½ hours for treatment is unusual
and not normal. Nurse 2 repeated that the Emergency Department was
understaffed.
The OIG team sought assistance with reading the Howard
Emergency Department medical record for the Doe because of illegible
handwriting. Nurse 2 was asked to read the “EMERGENCY PHYSICIAN RECORD
I” and “II” in order to inform the OIG team about the content of
the doctor’s notes. Nurse 2 could not read many of the notes, but knew
the writing belonged to Doctor 1. She stated that Doctor 1 is notorious
for her unreadable handwriting, and explained that, “No one can read
it.” Nurses must read doctor’s orders, which detail necessary
treatment for a patient.
Nurse 3 has been an registered nurse since 1996. She has
worked in various clinical areas at Howard since 1999, and began working
in the Emergency Department in 2002. Her shift is 7:30 p.m. to 8:00 a.m.
On January 6, Nurse 3 arrived at work at 8 p.m. and was
the team leader for the Blue Team. Sometime after 10 p.m., she noticed a
patient in the triage area with a lot of vomit on him. She asked the
triage nurse what was wrong with the patient, and the triage nurse told
her, “EMS noted ETOH.” Nurse 3 stated that she “left it alone”
and went back to work. The other nurse on her team, Nurse 4, was with a
trauma patient, so Nurse 3 was alone on the Blue Team.
Doctor 1 asked who was going to clean the patient in the
hallway, referring to the patient that Nurse 3 had seen in the triage
area earlier. Nurse 3 had not received any information from the charge
or triage nurse about this patient. Because he had not been able to give
his name, he was considered a “Doe.” The patient was fully dressed
and wrapped in a yellow FEMS blanket. The stretcher was in an upright
position, and the patient was slumped to one side with his eyes open. He
was covered with vomit but she did not notice a smell. According to
Nurse 3, “it looked like he had just eaten dinner.” Nurse 3 did not
perform an assessment because she had been told the patient was ETOH.
She assumed that was why the patient had vomited. The
patient was not in respiratory distress, so he “was not a priority at
that time.” The other Blue Team nurse came back to the Emergency
Department but had to deal with another patient. Thirty minutes after
she asked the first time, Doctor 1 asked again who would be cleaning the
patient. Nurse 3 responded, “When we get someone free, we will.”
At approximately 11:30 p.m., when the night shift was
arriving and after Nurse 4 was finished with his patients, Nurse 3 asked
him to help her clean the patient in Hallway D. Nurse 3 was going to put
a screen around the patient in the hallway and clean him up there, but
Nurse 4 wanted to put him in a room. Nurse 3 stated that she was pulling
the stretcher down the hall and noticed that the patient’s breathing
had changed to a “snoring” noise. It did not appear to be a sleeping
snore. She could tell his breathing had changed since her earlier
observation of him, and the change was “for the worse.” It did not
sound like shortness of breath. It was more like a growl. Nurse 4
performed a sternum rub, and the patient “flipped his arms and legs
inward.” She demonstrated this movement by rotating her arms and legs
inward toward her body.
Nurse 3 began to undress the patient by removing his
pants, and noticed that the back pocket of the pants was ripped or torn.
Nurse 3 did not notice any bruising on his body. Nurse 4 removed the
patient’s jacket. His clothes were put in a bag and moved with him.
Nurse 3 left his wedding ring on, but took off the watch and put it in
her pocket. Nurse 3 later gave the watch to a Surgical Intensive Care
Unit nurse. She stated that it was an expensive watch and she did not
want to leave it in the bag with his clothes.
Nurse 3 saw Nurse 4 repeat the sternum rub and the
patient responded with the same movements. They knew, based on this
response, that he probably had a head injury. Nurse 4 found a laceration
to the man’s head and went to get Doctor 1. Nurse 3 went to get IV
equipment and when she returned to the room less than 5 minutes later,
Nurse 4 and Doctor 1 were moving the patient to the resuscitation room.
By then, Nurse 4 or Doctor 1 had called the trauma team. Doctor 1
started to intubate67 the patient. Nurse 3 did an EKG.
Nurse 3 never saw the 151 Run Sheet or the triage form.
The OIG team sought assistance from Nurse 3 with reading the Howard
Emergency Department medical record for the Doe. She was asked to read
the “EMERGENCY PHYSICIAN RECORD I” and “II” in order to inform
the OIG team about the content of the doctor’s notes. The OIG team
showed her several documents with handwriting that she recognized as
Doctor 1’s, which she described as “terrible.” She tried to read
the writing but could not.
Nurse 4 has been a registered nurse and a staff nurse at
Howard Emergency Department for 2 years. His shift is 7:30 p.m. to 8:00
a.m.
On January 6, Nurse 4 arrived at work at 7:30 p.m. Nurse
3 was the team leader on the Blue Team. Nurse 4 took a patient to the
Intensive Care Unit, and when he returned to the Emergency Department,
another patient was assigned to him. Nurse 4 saw the patient in Hallway D, and Nurse 3 told him that
the patient was brought in for “ETOH.” The stretcher was upright so
the patient was sitting up. The patient’s eyes were closed, and he was
not talking. He was not actively vomiting and did not vomit at any point
while they were caring for him.
Doctor 1 had asked the nurses more than once to clean up
the patient in the hall so that she could examine him. Doctor 1 had
looked at the patient, but had not examined him. Nurse 4 and Nurse 3 put
the patient in Room 9. The patient was “nonverbal.” He had vomit on
his shirt. It was noticeable and hard to miss. Nurse 4 did not smell
alcohol. Before they moved the patient, he was breathing normally; then,
the patient began “snoring” respirations, which concerned Nurse 4
because some people snore when they have head trauma. Nurse 4 pinched
the patient and he evidenced “posturing.”68 Nurse 4 could not
believe it because he thought the patient was in the emergency
department for ETOH. Nurse 4 pinched him again, and the patient postured
again. Nurse 4 called out to Doctor 1 that the patient in Room 9 was
posturing, and Nurse 4 and Doctor 1 moved the patient to the
resuscitation room. Nurse 4 felt the back of the patient’s head and
found a small amount of blood in his hair. Nurse 4 found a small
laceration measuring 1 centimeter or less. Nurse 4 did not recall seeing
any bruising anywhere on the patient’s body.
When asked if he saw or completed any portion of the
triage form, Nurse 4 stated that he did not see the triage form before
he started caring for the patient. Consequently, he did not know the
patient’s vital signs or what priority level he had been assigned.
When shown the patient’s triage form, indicating the “Doe’s” low
temperature, Nurse 4 stated that a patient with such a low temperature
has to be warmed. In addition, an EKG should be performed. Nurse 4
stated that if he obtained that temperature reading, he would retake the
temperature. If a patient has low body temperature, he should be placed
in a room so that a rectal temperature can be obtained. If the patient
still has a low temperature, the nurse has to start warming the patient.
According to Nurse 4, intoxicated patients should be
considered a priority Level II, unless they need assistance with
respirations; otherwise, they can be a Level III. Even if FEMS personnel
say that a patient is intoxicated, the nurse is required to shake the
patient and make sure the patient is alert and awake. Even if patients
are sleeping, the nurse is required to wake them.
The OIG team sought Nurse 4’s assistance in reading the
Howard Emergency Department medical record for the patient. OIG team
members showed Nurse 4 several documents with handwriting that he
identified as Doctor 1’s, based on the signature. He tried to read the
writing but could not.
Nurse 5 is an Assistant Clinical Manager of the Emergency
Department. She has been a registered nurse since 1969 and a staff nurse
at Howard for 13 years. According to Howard’s guidelines, Nurse 5 functions as charge
nurse if there is a need for back up or if there is inadequate staffing.
Her shift is usually 3:30 p.m. to midnight.
On January 6, Nurse 5 was charge nurse until 7:30 p.m.,
when Nurse 2 arrived and took over. Nurse 5 then took over as ambulance
triage nurse. According to Nurse 5, EMTs bring a patient in, get them
triaged, complete the 151 Run Sheet, and then take it to the triage
nurse to be signed. Nurse 5 assessed an ETOH patient in the ambulance
triage area who had a bandage on his head. He was sitting and talking on
the end of a stretcher. She sent him to the waiting room.
Between 10 and 10:15 p.m., Nurse 5 decided to take a
break and told Nurse 1, “If it’s not that busy, cover ambulance
triage.” Nurse 5 ate and headed for her office to do some paperwork.
On her way to her office, Nurse 5 saw an EMT pushing a patient down the
hall to Hallway D. The patient was sitting upright, but slumped with his
head to the side. He had vomit on him.
Nurse 5 returned to the ambulance triage area, where
there were four to five ETOH patients waiting. A white male EMT (EMT 2)
handed her a 151 Run Sheet. Nurse 5 stated that she did not read it
because the EMT told her it was for “the ETOH patient you just did.”
She took that to mean the man with the bandage on his head whom she had
triaged earlier and sent to the waiting area. Nurse 5 stated that she
signed and dated the 151 Run Sheet without reading it.
The night was very busy. Nurse 5 was leaving at the end
of her shift and saw Nurse 3 putting on a disposable hat and gown so she
could clean the patient with vomit on him. Nurse 3 was preparing to take
the man into a room, and Nurse 5 asked if she needed help. Nurse 3 said,
“No,” because Nurse 4 was going to help her.
Nurse 5 was off on January 7 and 8. When she returned to
work on January 9, she was told that she had signed a 151 Run Sheet for
the “Doe” who turned out to be Mr. Rosenbaum. Nurse 5 stated that
she initially said, “No, I didn’t.” After being shown the 151 Run
Sheet by a Howard official, she said, “Sure enough, I signed it.”
The OIG team showed Nurse 5 the triage form for the
“Doe,” and Nurse 5 stated she had never seen it. She stated that if
a patient had that same low temperature, she would recheck the
patient’s temperature or take it rectally. Nurse 5 would let the
doctor know about the low body temperature, and start warming the
patient. According to Nurse 5, Emergency Department nurses do not have
to wait for doctors to tell them to go to the next step in treating a
patient. In addition, an ETOH patient is supposed to get a neuro check.
After reviewing the triage form, Nurse 5 stated that she would have
considered this patient a Level II who needed immediate intervention.
She would not have considered him a Level III. A Level III designation,
which Nurse 1 had assigned to the patient, allows patients to be seen
within 2 hours or as soon as possible.
The OIG team showed Nurse 5 the 151 Run Sheet for the
patient later identified as Mr. Rosenbaum. Nurse 5 said that if she had
read it on January 6, she would have questioned it. She stated a GCS of less than 8 requires
that EMTs call the hospital to advise them that they are bringing in
this patient.
Nurse 5 looked at Emergency Physician Record I, but could
not read most of the writing. She could only read “cc:” and
“unable to obtain.” Nurse 5 stated that Doctor 1’s handwriting is
“terrible.” Nurse 5 also stated that she has to ask Doctor 1 what
she has written on a document and then must write it separately in her
own handwriting so that she can read it.
Doctor 1 has been a medical doctor for 8 years. She has
been an Assistant Clinical Professor at Howard since June 2002. In
addition, Doctor 1 works full-time as an Emergency Department physician
where she schedules the medical staff for their shifts. There are 27
Emergency Department full-time physicians, and some part-time
physicians.
An Emergency Department physician’s start time
determines to which team, Red or Blue, they are assigned. The arriving
physician relieves one who is completing a shift. Doctor 1 believes she
worked the 4 p.m. to 1 a.m. shift on January 6. Even though the shift
ends at 1 a.m., “they usually leave early, as soon as the 12 midnight
person gets there, and they are all set.” Doctor 1 remembered January
6 as a “moderate night,” with nursing staff “probably short.”
There were only two nurses on the Blue Team. Doctor 1 remembers that
Doctor 2 was working in the Emergency Department that evening and was
assigned to the Red Team.
Doctor 1 stated that a male Caucasian came in a “yellow
bag” with vomit all over his face and his chest. The “bag” was an
FEMS blanket. FEMS usually uses this bag to keep the person warm or if
they have body fluids on them. Doctor 1 described the man as “very
disheveled, unkempt, his hygiene wasn’t the best. He looked dirty. He
looked like our typical alcoholic.”
Doctor 1 asked the nurse why the patient in Hallway D was
there, and the nurse told her “ETOH.” Doctor 1 performed a “brief
focused exam” at around 11 p.m. that consisted of “head to toe,
heart, lungs, pupils.” Doctor 1 did not find any hematoma, swelling,
or injury to the patient’s head after performing this head to toe
examination. Doctor 1 stated that the patient’s pupils were “fine”
at that time; they were “normal reaction.” She listened to his lungs
through his clothed chest. Doctor 1 stated that the patient smelled like
alcohol.
When the OIG team asked Doctor 1 about the patient’s
clinical presentation (e.g., slumped, unresponsive, not talking), Doctor
1 stated, “It doesn’t tell me anything. It tells me he has been
drinking. I saw an unresponsive person who didn’t respond like a
person who is drunk.” She stated she did “noxious stimuli.” When
asked to clarify what that means, she stated, “I pinched his nipples
and he grimaced.”
Doctor 1 stated that she told the nurses to put the
patient in a room and undress him. She stated that while she was at the
nursing station, she saw the patient posturing as the nurses were taking his clothes off. Doctor 1 knew
right away that posturing was a bad sign. She stated that posturing is a
sign of “intracranial insult,” and that, “I have a patient like
this every shift. I intubate them and they leave with vital signs.”
The patient needed breathing assistance. Consequently,
they took him to the resuscitation room so Doctor 1 could intubate him.
Doctor 1 stated that if she did not intubate the patient right away, he
would die. “You want to decrease the pressure to the brain.” It is
her practice to move a patient to the resuscitation room because it is a
larger room and better equipped for emergency care. When Doctor 1
intubated the patient, she noted that he had a hematoma. She then called
for the trauma team.
Doctor 1 estimated that from the first time she saw him
until the posturing in Room 9 was 15-20 minutes. She did “a more
complete exam” and saw that his pupils now were unequal and sluggishly
reactive. The patient’s breathing was shallow. When asked if he was
pale, Doctor 1 stated, “I am not a good judge of that. He looked like
most Caucasians.” Doctor 1 did not note any bleeding or any trauma to
his body. She noted a small bump on the right side of his head; it was
quarter sized and “just slightly stuck out from his head.”
When asked about the GCS, Doctor 1 said she never does it
because it is a very complicated test and she does not have time to do
all the calculations necessary. She stated, “you have to write the
numbers next to everything.” Doctor 1 explained the GCS by stating
that a result of 6-8 means that a person can move one side. Less than
that means a person cannot move at all. With a result of 14, the person
would wake up. She stated that she likes the AVPU test69 better because
it is more accurate.
Doctor 2 is a part-time Emergency Department physician at
Howard who works a 10 a.m. to 10 p.m. shift, 3-5 times per month. Doctor
2 began working at Howard in October 2002. He also works at Providence
Hospital part-time in the Emergency Department.
In addition to working at the hospitals, Doctor 2 is
employed as the Acting Medical Director for FEMS. As Acting Medical
Director, he is responsible for creating and updating patient care
protocols, reviewing 151 Run Sheets and other documentation, interacting
with FEMS employees, and overseeing medical quality assurance and other
patient care issues, including investigations of protocol violations.
On January 6, Doctor 2 was working at Howard Emergency
Department on the Red Team. Doctor 2 stated that January 6 was busy but
not any busier than any other night. Doctor 2 remembers Doctor 1, the
physician for the Blue Team, saying she needed help with a patient. In
response, after ensuring that his own patient in the resuscitation room
was stable, Doctor 2 pulled his patient from the room. He then helped
place Doctor 1’s patient in the resuscitation room. Doctor 2 described
the room as equivalent to an operating room in terms of size, equipment,
and lighting.
Doctor 2 assisted in rolling Doctor 1’s patient on his
side in order to place a long spine board underneath him. According to
Doctor 2, the patient was fully dressed when he saw him. When asked if
he saw any injuries to the patient, Doctor 2 stated that he noticed that
the patient “did not have much bruising.” He saw only a
quarter-sized bump on the back of the patient’s head and only because
of the floodlights that are located in the resuscitation room.
When Doctor 2 was asked if he leaves his shift early, he
replied that he does not. This contradicts Doctor 1’s assertion that
all physicians leave their shifts early. Doctor 2 said he had several
critical patients under his care and said he did not leave them until he
was sure they were stable and their care has been fully assumed by the
next person on duty. In addition, Doctor 2 had paperwork to complete.
Doctor 2 did not learn until after he assisted Doctor 1
that her patient had been transported to Howard by FEMS. Doctor 2
reviewed the 151 Run Sheet and noticed it had not been completed. He
called the FEMS on-duty supervisor and advised that all FEMS personnel
involved in the Gramercy Street call needed to write special reports
right away. Doctor 2 ordered Ambulance 18 out of service. It is standard
procedure to take a unit out of service for any matter in which a
special report is needed.
Doctor 2 did not participate in the FEMS investigation of
the Gramercy Street incident because he had been in the Emergency
Department at Howard on January 6, 2006, and had contact with the
patient involved in the matter. Doctor 2’s involvement was limited to
requiring special reports from all FEMS personnel involved and placing
Ambulance 18 out of service. A D.C. Department of Health physician
participated in the FEMS interview panel.
Doctor 2 reviewed the 151 Run Sheet for the Gramercy
Street patient. Doctor 2 believed that EMT 2’s GCS assessment was not
accurate. According to Doctor 2, localized movement (removing the oxygen
mask), spontaneous eye opening, and verbal responses (moaning) should
have resulted in a higher GCS score. Doctor 2 would have scored the
patient at a 13. Doctor 2 stated that he does not rely on the EMTs’
scoring on the GCS because “they do it wrong.”
- Critical patient assessments not
performed. The triage nurse, Nurse 1, did not properly assess the
patient presented to her. She relied on the FEMS assessment of the
patient’s clinical signs and did not perform basic assessments that
could have indicated the serious nature of his injuries. For example,
she did not do a pupil test, which is a basic test relied upon to
indicate brain function and consciousness. In addition, she obtained a temperature reading which was critically low, yet did
nothing to reassess the patient or communicate this abnormal finding
other than to circle the temperature reading on the triage form.
- Triage policy for intoxicated
patient not followed. Although Mr. Rosenbaum was incorrectly
characterized as an intoxicated patient (ETOH), Nurse 1 did not follow
the policy and algorithm for assessing a patient with alcohol
intoxication in order to determine the level of care necessary. Nurse 1
incorrectly categorized the patient as Level III, despite abnormal vital
signs. This categorization violated hospital policy on treating alcohol
intoxication, which classifies such patients as Level II. Nursing staff
that assumed care of the patient relied on the triage nurse to make a
correct assessment of the patient in order to prioritize patient care
management.
- Triage form inaccurate. Nurse 1’s
documentation inaccurately represented the patient’s level of
consciousness as awake and alert. As a result, caregivers who received
the form from her had misinformation about the patient’s mental
status.
- Charge nurse failed to review triage
form. The Charge nurse, Nurse 2, did not review the triage form given to
her by Nurse 1. Nurse 2 did not note the subnormal temperature, the
patient’s (incorrect) level of consciousness, and that the patient was
designated as a “Doe.” Nurse 2 also did not note that Nurse 1 had
designated the patient as a Priority III, in violation of hospital
triage policy.
- Triage form information not conveyed
to staff. Nurse 2 failed to convey information about the patient to Blue
Team nurses. She incorrectly believed that Nurse 4, who was busy with a
trauma patient, was the team leader rather than Nurse 3. Consequently,
Blue Team nurses were not aware of the patient’s abnormal vital signs
and altered mental status and, as a result, did not immediately assess
or care for the patient, or call for physician intervention.
- 151 Run Sheet signed without review.
The Assistant Clinical Manager, Nurse 5, failed to review the 151 Run
Sheet, but signed the form as the “person receiving patient.” Nurse
5 apparently thought that this was the Run Sheet for another ETOH
patient who was alert and talking. The 151 Run Sheet she signed,
however, described a patient with a low GCS, abnormal vital signs, and
repeated vomiting—all signs of a serious medical condition. As the
Assistant Clinical Manager, she should have ensured that the patient
whose run sheet she signed was appropriately prioritized and treated.
- Standard of care not followed.
Howard “Patient Care Standards,” “Standard of Care: Care of the
Patient with Alcohol Intoxication” was not followed by any of the
nurses in the Emergency Department. The standard includes directives to:
“assess and monitor airway and breathing, assess for evidence of trauma, notify MD of the patient’s condition if
unstable … obtain routine labs … monitor vital signs every 15
minutes … until stable, perform neuro checks every 30 minutes until
stable ….” None of these care standards was followed. Although
alcohol intoxication was not a correct diagnosis or valid assessment of
the patient’s condition, it was the diagnosis that the nurses
accepted. Therefore, that diagnosis should have dictated how they
provided care.
- Physician’s poor handwriting
impeded nurses’ ability to read documentation. Emergency Department
staff complained consistently that Doctor 1’s handwriting is extremely
difficult to read. When the OIG team told her about this complaint, she
stated that she can read her writing, and if someone has a question
about what she has written, they could come and ask her. Doctor 1 said,
“They work with me, they must can read it. People ask me to interpret
if they can’t read it.” She stated that nurses follow order sheets,
so they do not have to read the Emergency Physician Record. The OIG team
could not read Emergency Department documents written by Doctor 1
related to Mr. Rosenbaum’s care and had to ask her to decipher the
writing. For example, the Emergency Physician Record I, “Chief
Complaint,” section is not legible. When shown the document, Doctor 1
read it for the interviewers, indicating that the text noted the
patient’s mental status and that his HPI70 could not be obtained, he
was uncommunicative, and he had vomit on his clothing.
- Doctor 1’s recollection of her
actions not supported. Ambulance 18’s patient was signed in at Howard
at 10:30 p.m. Doctor 1’s interview statements indicated that she
assessed the patient much earlier than documented in the Emergency
Department Record and reported by nursing personnel. For example, Doctor
1 stated that she initially examined the “Doe” in Hallway D at
approximately 11 p.m. However, on the Emergency Physician Record I that
she completed, Doctor 1 indicated that she saw the patient 45 minutes
later. The OIG team showed this document to Doctor 1. She stated that
despite the fact that she had written a different time in the “TIME
SEEN” section of the form, she actually saw the patient at 11 p.m.
There is an additional discrepancy between Doctor 1’s
interview statements and Howard’s written documentation. Doctor 1
stated that she saw the patient and ordered lab tests and IV fluids at
11 p.m. However, her written notations describe her examination and her
orders for the patient occurring 50 minutes later. Nursing documentation
indicates that they complied with the orders at 12 a.m. and thereafter.
Doctor 1 stated to the OIG interviewers that she saw the
patient at 11 p.m., and 15-20 minutes later, she noted posturing,
intubated him, and called the trauma team. Medical documentation,
however, indicates that vital signs, IV, and other interventions were not initiated until
approximately 12:00 a.m. and that the patient was intubated after 12:00
a.m. The trauma team signed on to take over the patient’s care at
12:15 a.m.
- That Howard develop a color coding or other system
that will enable staff to readily identify the priority level of
patients awaiting care in the Emergency Department hallways. In Mr.
Rosenbaum’s case, there was no indicator on his stretcher or on his
person to inform a passing caregiver about his assigned priority level.
- That Howard consider adopting a patient records system
that would enable nursing and medical staff to review documents when
they are at a patient’s side. The current system, which maintains
Emergency Department documents in a chart rack far removed from patient
locations, prevents staff from gaining information regarding a
patient’s status in a timely manner. For example, the nurses and the
physician passed Mr. Rosenbaum in the hallway several times, but had no
ready access to information regarding his altered mental status,
subnormal temperature, or pre-hospital condition.
The OIG team interviewed the Deputy Chief Medical
Examiner, who conducted the autopsy on Mr. Rosenbaum. The Deputy Chief
Medical Examiner has worked at OCME since 2001.
The Rosenbaum autopsy began on January 10, 2006, and
concluded on January 13. The Deputy Chief Medical Examiner indicated
that the autopsy produced some significant findings. The Deputy Chief
Medical Examiner described how a pattern of injury to the brain
indicates what happened to cause the injury.
The Deputy Chief Medical Examiner stated that the
patient’s vomiting was an important sign that should have alerted
medical personnel that there was a brain injury. The very low Glasgow
Coma Scale was another indicator that there was a serious injury.
The initial interview was not completed because some of
the autopsy photographs, which had been taken with a 35 mm camera, had
not been developed into slides. The team viewed all of the slides except
those of Mr. Rosenbaum’s brain. Consequently, the OIG team arranged a
return visit to OCME on March 27 to review the entire set of slides from
the Rosenbaum autopsy. The team asked to view the complete set of slides
in order to select some for duplication. The team wished to show
photographs of Mr. Rosenbaum’s injuries to the various health and
emergency care providers who had contact with Mr. Rosenbaum to determine
when his injuries first became noticeable. However, the Deputy Chief
Medical Examiner stated that that some slides were not immediately
available because they had apparently been misfiled in another
decedent’s record. Later, the Deputy Chief Medical Examiner advised
the OIG team that OCME technicians had not located the slides. The
Deputy Chief Medical Examiner stated that she would look for the slides
herself and advise the OIG team when they were located. To date, the
slides have not been provided.
- The OCME conducted the autopsy
expeditiously and issued a report soon thereafter.
- At the time of the OIG team’s
interview with the Deputy Chief Medical Examiner, OCME was not using
digital photography, which would allow fast and easy electronic storage,
retrieval, and duplication of autopsy photographs. The film-based
technology being used prevented ready access to the entire set of
autopsy photographs sought by the OIG team because of the need to send
the film out for processing. In addition, duplicated prints and slides
can be misfiled and difficult to locate, as happened in this case.
That the OCME consider using digital camera technology to
photograph all autopsies to improve the processing speed, accessibility,
and retrieval of autopsy photographs. The OIG team was unable to review
requested autopsy photographs because of photo processing delays and
mislaid slides.
The OIG team concludes that personnel from the Office of
Unified Communications properly monitored the 911 call from Gramercy
Street and immediately dispatched adequate resources to respond to the
emergency. However, FEMS, MPD, and Howard personnel failed to respond to
David E. Rosenbaum in accordance with established protocols. Individuals
who played critical roles in providing these services failed to adhere
to applicable policies, procedures, and other guidance from their
respective employers. These failures included incomplete patient
assessments, poor communication between emergency responders, and
inadequate evaluation and documentation of the incident. The result,
significant and unnecessary delays in identifying and treating Mr.
Rosenbaum’s injuries, hindered recognition that a crime had been
committed.
On January 6, 2006, David E. Rosenbaum consumed alcohol,
both before and during dinner prior to leaving home for a walk.
Neighbors discovered Mr. Rosenbaum lying on the sidewalk in front of
their home and called 911. Upon assessment, emergency responders
concluded that Mr. Rosenbaum’s symptoms, which included poor motor
control, inability to speak or respond to questions, pinpoint pupils,
bleeding from the head, vomiting, and a dangerously low Glasgow Coma
Scale, were the result of intoxication. Hospital laboratory and other
tests, however, confirmed that Mr. Rosenbaum’s symptoms were caused by
a head injury. Emergency responders’ approach to Mr. Rosenbaum’s
perceived intoxication resulted in minimal intervention by both medical
and law enforcement personnel.
FEMS personnel made errors both in getting to the scene
and in transporting Mr. Rosenbaum to a hospital in a timely manner.
Ambulance 18 did not take a direct route from Providence Hospital to the
Gramercy Street incident. In addition, for personal reasons, the EMTs
did not take the patient to the nearest hospital. Because of that
decision, it took twice as long for Ambulance 18 to reach Howard than it
would have taken to get to Sibley Hospital. Once FEMS personnel at the
Gramercy Street scene detected the odor of alcohol, they failed to
properly analyze and treat Mr. Rosenbaum’s symptoms according to
accepted pre-hospital care standards. Failure to follow protocols,
policies, and procedures affected care of the patient and the efficiency
with which the EMTs completed the call. In addition, FEMS employees’
failure to adequately and properly communicate information regarding the
patient affected subsequent caregivers’ abilities to carry out their
responsibilities.
MPD officers initially dispatched in response to the
Gramercy Street call failed to secure the scene, collect evidence,
interview all potential witnesses, canvass the neighborhood, conduct
other preliminary investigative activities, or properly document the
incident. Both FEMS and MPD failures were later compounded by similar
procedural failures on the part of Howard Emergency Department
personnel, who also initially believed Mr. Rosenbaum’s condition to be
the result of intoxication.
Upon Mr. Rosenbaum’s arrival at Howard, Emergency
Department personnel failed to properly assess his condition and failed
to communicate critical medical information to each other, thereby
delaying necessary medical intervention, all in violation of Howard’s
own patient care standards. Further, a number of Emergency Department
staff members passed Mr. Rosenbaum in the hallway and neglected to
provide clinical and therapeutic care.
The Office of the Inspector General’s review indicates
a need for increased oversight and enhanced internal controls by FEMS,
MPD, and Howard managers in the areas of training and certifications,
performance management, oral and written communication, and employee
knowledge of protocols, General Orders, and patient care standards.
Multiple failures during a single evening by District agency and Howard
employees to comply with applicable policies, procedures, and protocols
suggest an impaired work ethic that must be addressed before it becomes
pervasive. Attitudes of apathy, indifference, and complacency—apparent
even during some of our interviews with care givers—undermined the
effective, efficient, and high quality delivery of emergency services
expected from those entrusted with providing care to those who are ill
and injured.
Accordingly, while the scope of this review was limited,
these multiple failures have generated concerns and perceptions about
the systemic nature of problems related to the delivery of basic
emergency medical services citywide. Such failures mandate immediate
action by management to improve employee accountability. Specifically,
we believe that several quality assurance measures may assist in
reducing the risk of a recurrence of the many failures that occurred in
the emergency responses to Mr. Rosenbaum: systematic compliance testing,
comprehensive and timely performance evaluations, and meaningful
administrative action in cases of employee misconduct or incompetence.
Interviewees Contradictory Statements
The OIG team noted multiple discrepancies in statements
made by interviewees. Not only did some statements on the same subject
differ from person to person, but also, in some instances, statements
made to the OIG team differed from what interviewees told FEMS, MPD, and
DOH reviewers.
- Smell of alcohol. Neighbors 1 and 2 stated that they did
not smell any alcohol on Mr. Rosenbaum. All of the firefighters claimed
to have smelled alcohol. The MPD officers stated they did not get close
enough to Mr. Rosenbaum to smell alcohol. EMT 2 stated that “the
patient’s vomit did not smell like anything.” EMT 1 stated that she
did not get close enough to the patient to smell alcohol. EMT 1 also
stated that when she cleaned Ambulance 18, she smelled neither vomit nor
alcohol. The Howard Emergency Department triage (Nurse 1) stated that
the patient’s vomit smelled like alcohol. Emergency Department Nurse 4
stated that he did not smell alcohol. Howard physician Doctor 1 stated
that she smelled alcohol.
- Patient vomiting. Neighbors 1 and 2 stated that Mr.
Rosenbaum started vomiting when the firefighter/EMTs administered
oxygen. FF/EMT 1 stated that there was vomit on Mr. Rosenbaum when
Engine 20 arrived. FF stated that Mr. Rosenbaum starting vomiting after
they arrived and treatment started.
- Patient bleeding. When FF was
interviewed by the FEMS Interview Panel on January 18, he did not
mention any use of gauze in treating Mr. Rosenbaum. He initially told
the OIG team that FF/EMT 2 or FF/EMT 1 used gauze on the back of Mr.
Rosenbaum’s head. FF then stated that his colleagues only used gauze
pads to clean the vomit from the patient’s face. FF/EMT 2 told the
FEMS Interview Panel that he did not observe any injuries or bleeding on
the scene. He told the OIG team, however, that he placed a 4x4 gauze pad
on the patient’s head, and applied pressure that stopped the minimal
bleeding. All three MPD officers stated to the OIG team that they saw
firefighter/EMTs holding a white bandage to the back of the patient’s
head. Officer 2 described seeing blood on the bandage.
- Patient’s ability to sit up.
FF/EMTs 1 and 2 and FF told the FEMS Interview Panel that Rosenbaum
could sit unassisted. However, they all told OIG team that the patient
was propped up against FF/EMT 1’s legs. FF/EMT 1 said they took turns
holding him up in a sitting position.
- Patient’s vital signs. FF stated
that FF/EMT 2 or FF/EMT 3 gave the female EMT (EMT 1) the patient’s
vital signs, which had been written on one of the firefighter’s
gloves. FF/EMT 2 stated that he wrote both his and FF/EMT 3’s vital
signs readings on a piece of paper which he gave to FF/EMT 3. FF/EMT 3,
however, stated that FF/EMT 2 wrote the vital sign readings on a glove.
EMT 2 stated that he received an oral report of one vital signs reading
from FF/EMT 3, but received no written report on vital signs from any of
the first responders. EMT 1 stated none of the firefighters were wearing
gloves, and no one gave her any medical information.
- Lower body assessment. FF/EMT 2 stated that FF/EMT 1
performed an assessment of the patient’s lower body. FF/EMT 1,
however, denied doing any assessment of the patient. He stated that he
concentrated on giving him the oxygen and that “was hard enough.”
- Crime suspicions not mentioned to
FEMS Interview Panel. During his interview with the OIG team, FF/EMT 3
stated that he had expressed suspicions to his colleagues in the
presence of a MPD officer that Rosenbaum, who had no wallet or ID, had
been robbed. FF/EMT 3 told the OIG team that his colleagues agreed with
him, and the MPD officer standing nearby “just shrugged.” Neither
FF/EMT 3 nor the other firefighters gave this information to the FEMS
Interview Panel.
- MPD officer activities. Officer 3
gave the OIG team differing versions regarding her arrival at the
Gramercy Street call: she first stated that Officers 2 and 1 arrived
before she did. She later stated that she saw them arrive. Officers 1
and 2 stated that Officer 3 was at the scene when they arrived.
According to the MPD General Order “Field Reporting System,” the
first officer on the scene, regardless of assignment, must conduct the
preliminary investigation. Officer 3 stated to the OIG team that she
interviewed the male neighbor who called 911. Officer 1 stated to the
OIG team that Officer 3 interviewed Neighbor 1. Officer 1’s signed and
sworn statement to the MPD Second District investigator regarding this
incident, however, indicates that Officer 3 only talked to the Engine 20
personnel regarding the identification of the man down. Two of the
Engine 20 personnel, FF and FF/EMT 3, agreed that Officer 3 stayed in
her vehicle after she arrived. Neighbor 1 stated that he was interviewed
by a male MPD officer, and he did not see or talk to a female MPD
officer at the Gramercy Street scene.
- Physician’s description of patient at variance with all
other accounts. All persons interviewed by the OIG team indicated that
Mr. Rosenbaum was neatly dressed and “looked like he belonged in the
neighborhood.” He was wearing a watch and jewelry. Doctor 1, however,
described the patient as “very disheveled, unkempt; his hygiene
wasn’t the best. He looked dirty. He looked like our typical
alcoholic.”
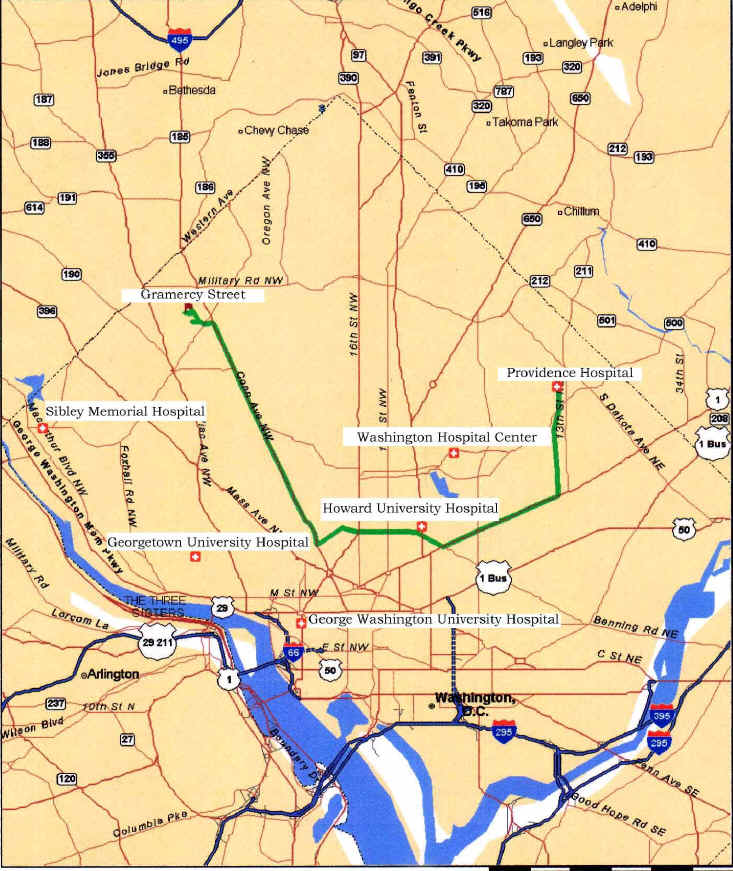
AMBULANCE 18 from PROVIDENCE HOSPITAL to GRAMERCY STREET
Not available online.
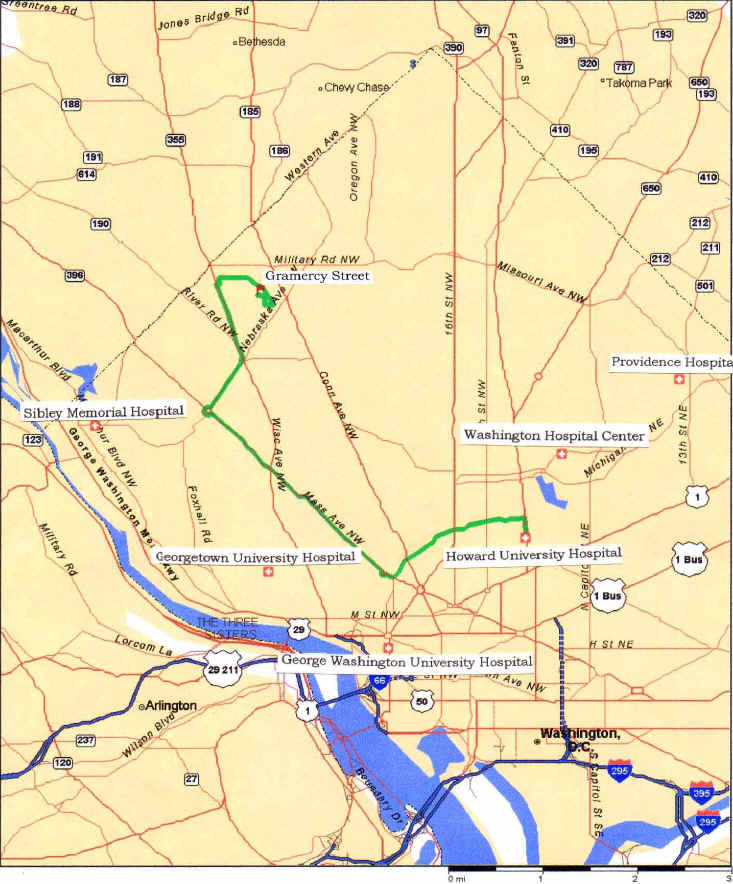
AMBULANCE 18 from GRAMERCY STREET to HOWARD HOSPITAL
Not available online.
1 FEMS and MPD also conducted inquiries into the actions
of their responders to the Gramercy Street emergency. In addition, the
District’s Department of Health conducted a “complaint
investigation” into Howard University Hospital’s response.
2 The care and treatment provided to Mr. Rosenbaum at
Howard University Hospital subsequent to the discovery of his head
injury, and the MPD assault and robbery investigation that was opened on
January 7, 2006, were not part of the Inspector General’s review.
3 Emergency response by fire and ambulance personnel.
4
Heartbeat, breathing, and blood pressure.
5 The process of sorting out and classifying patients to
determine the priority of needs and where a patient should be treated.
6 Medical Priority Dispatch System Software (ProQA).
7 Alpha and Bravo are non-critical medical calls. Alpha
calls are handled by a Basic Life Support unit. Bravo calls are handled
by a first responder and a Basic Life Support unit. Charlie and Delta
are critical medical calls requiring first responder and Advanced Life
Support response.
8 An engine company has a smaller truck with hoses. A
truck company has the larger hook and ladder fire truck.
9 First responders who provide the most extensive
pre-hospital care, and have advanced training that allows them to
perform more complicated treatments, such as administering IV fluids and
drugs, interpreting EKGs, and performing endotracheal intubations.
10 Ambulances have standardized equipment, layout, and
capacities. A Basic Life Support ambulance is upgraded to an ALS
ambulance when paramedics carry equipment on board that they have
special training to use.
11 A first responder trained to provide basic emergency
pre-hospital care and to transport patients by ambulance to a hospital.
EMTs have the skills to assess patient condition and manage respiratory,
cardiac, and trauma emergencies.
12 A face mask and bag device that delivers high
concentrations of oxygen.
13 A device that delivers low concentrations of oxygen
through prongs that rest in the nostrils.
14 Includes DANIEL LIMMER & MICHAEL F. O’KEEFE,
EMERGENCY CARE, (2005).
15 EMT-Advanced skill.
16 EMT-Advanced skill.
17 EMT-Advanced skill.
18 Status levels are: alert, responds to verbal stimuli,
responds to painful stimuli, and unresponsive.
19 “Note Well” is printed in a highlighted area
marked with a bold triangle containing an exclamation point, meant to
designate an issue of special importance.
20 Except for ambulance patients.
21 Problem-solving procedures.
22 Fainting.
23 A computer-generated, chronological log that documents
the activities associated with 911 calls, based on the exchange of
communication between the Office of Unified Communications and the fire,
police, and emergency response units in the field.
24 These firefighters are referred to as “firefighter/EMTs."
25 The actual time the call was received was 9:30 p.m.
26 Prior to interviewing FEMS personnel, the OIG team
interviewed MPD officers who stated that they had seen the firefighter/EMTs
using gauze on the back of the patient’s head.
27 Ethyl Alcohol: the alcohol in wine, whiskey, and other
spirituous beverages.
28 FF/EMT 2 is an EMT-Advanced.
29 A form of physical stimulus used to check for
consciousness, performed by rubbing knuckles against the patient’s
sternum (the breast bone).
30 To examine by feeling and pressing with the palms and
fingers of the hand.
31 A high-powered flashlight.
32 Extremely contracted.
33 See D.C. Adult Pre-Hospital State Medical
Protocols, Skills Procedures, Oxygen Administration Chart at J16.1.
34 See DANIEL LIMMER & MICHAEL F. O’KEEFE,
EMERGENCY CARE, 687-88 (2005).
35 A computerized, comprehensive chronology of all FEMS
and MPD dispatch communication for a specific incident.
36 A union representative attended the OIG interviews
with the MPD officers.
37 Later in the interview, Officer 3 contradicted this
statement by stating that she saw the unit 2021officers arrive.
38 PD Form 251 (Event Report) is to be used for
documenting reported incidents or offenses.
39 EMT 1 attended the OIG interview accompanied by a
union representative.
40 EMT 1 paused during the interview to ask the union
representative what street Providence Hospital was on. The OIG team did
not permit the representative to answer EMT 1.
41 Low priority.
[Footnotes 42 and 43 not in original report.]
44 Upon acknowledgement by an emergency responder that it
has been dispatched to a call, Communications considers the unit to be
“en route.” FEMS personnel are required to use the DEK to confirm
their en route status.
45 According to the vehicle tracking system used by FEMS,
the route taken by EMT 2 and EMT 1 was 12th Street to Rhode Island
Avenue, Rhode Island Avenue to Florida Avenue, Florida Avenue to
Connecticut Avenue, Connecticut Avenue to Fessenden Street, Fessenden
Street to Huntington Street, and Huntington Street to Gramercy Street.
46 According to the vehicle tracking system used by FEMS,
the route taken by EMT 2 and EMT 1 was Gramercy Street to 39th Street,
39th Street to Fessenden Street, Fessenden Street to Reno Road, Reno
Road to Jenifer Street, Jenifer Street to Wisconsin Avenue, Wisconsin
Avenue to Nebraska Avenue, Nebraska Avenue to Massachusetts Avenue,
Massachusetts Avenue to Florida Avenue, Florida Avenue to Barry Street,
and Barry Street to Georgia Avenue.
47 The official FEMS form used to document all aspects of
an emergency medical call.
48 A scale that assesses the response to stimuli in
patients with head injuries. The areas of assessment are eye-opening,
motor response, and verbal response.
49 Unstable patients.
50 Per www.mapquest.com.
51 A simple assessment of whether a patient’s blood is
circulating well, which is done by pressing the patient’s fingernail
and counting the time it takes for normal color to return after release.
52 A procedure for measuring the concentration of oxygen in the blood.
53 According to the Communications CAD system, Ambulance
18 was closer to Sibley (2.84 miles), Georgetown (3.52 miles), and
George Washington (4.62 miles) hospitals than to Howard (4.69 miles).
Washington Hospital Center, which is also closer than Howard, was closed
to ambulance patients. According to MapQuest, driving time from Gramercy
Street to Sibley is 7 minutes, and to Howard, 15 minutes.
54 Of note, the OIG team’s review of Ambulance 18’s
log entries revealed a derogatory comment regarding an intoxicated
person. The same EMTs who responded to the Gramercy Street call on
January 6, were also on duty the night a log entry was recorded in which
another patient was described as “drunk and stupid.” (See Appendix
5)
[Footnotes 55-58 are missing in the original/]
59 This form is the beginning of the patient record in
the Emergency Department, with a top section for the triage nurse to
complete, detailing information such as the patient’s name, sex, DOB,
date, time in, level of care, allergies, medications, past medical
history, vital signs, narrative assessment, means of arrival, and
referral site.
60 Persons whose identities are not known.
61 Underarm area.
62 Body temperature can be taken by oral, axillary, or
rectal means.
63 All other Howard Emergency Department interviewees
denied that Mr. Rosenbaum was covered with a Howard blanket.
64 A measure of oxygen concentration in the blood.
65 Howard University Hospital triage policy designates
alcohol intoxication as Level II, requiring that patients receive
immediate intervention after triage.
66 Check of the pulses far away from the center of the
body, motor function, and sensation.
67 Insertion of a tube to assist breathing.
68 Abnormal body position of two main types, both of
which imply severe damage to the brain with a need for immediate medical
attention.
69 Alert, Verbal response, Painful response,
Unresponsive. A test used to classify a patient’s level of
consciousness or responsive mental status from most to least reactive.
70 History of Present Illness.
|
![]()